Sun, Feb 8, 2026
[Archive]
1- Health Management and Social Development Research Center, Golestan University of Medical Sciences, Gorgan, Iran
2- Health Management and Social Development Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,Alirezaheidari7@gmail.com
2- Health Management and Social Development Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,
Full-Text [PDF 457 kb]
(308 Downloads)
| Abstract (HTML) (2173 Views)
Discussion
Based on the present study, the patients’ trust in physicians in both Sayyad Shirazi and 5 Azar Gorgan hospitals was determined to be at an optimal level. This rate was lower compared to the studies of Hall et al. (22) and Foraty et al. (24). Even though the result may be due to the high trust of the patients in physicians as a result of appropriate medical services and the high skill of physicians, patients admitted to medical teaching hospitals mostly include individuals with lower financial ability who may have lower expectations of medical services and higher trust in physicians. It seems that the expenses incurred in recent years, resulting from spending the funds of the Health Transformation Plan to purchase advanced medical equipment, renovate and improve the physical space of hospitals, and enhance care due to the increase in nursing manpower during the peak of the COVID-19 pandemic, are a confounding factor in measuring patients' trust in physicians. It should also be kept in mind that, despite emphasizing the confidentiality of the questionnaire information and its lack of impact on the treatment process, some patients may not have answered honestly.
The absence of a significant relationship between the trust score and background and demographic variables in the present study is largely consistent with the findings of Graham et al.'s study. In their study, there was no significant relationship between gender, race, and education with trust in the physician. The findings of Englehart et al.'s study, mentioning no significant relationship between demographic variables such as age, marital status, and education level with their level of trust, are consistent with the findings of the current study (25). The findings of Kim et al.'s study are in some respects consistent with the findings of the current study. In the mentioned study, no significant relationship was found between age, education, place of residence, type of insurance, and home ownership with trust in the physician. However, the study showed a significant relationship between the variables of income and gender and the level of trust in the physician, such that as income decreased, the level of trust in the physician also decreased, and female patients had 0.67 less trust in physicians than men (26). Zarei et al. observed no significant relationship between patients' trust in physicians and variables such as age, sex, and education, which is in accordance with the results of the current study. However, findings such as a significant relationship between covered insurance and trust in physicians are contrary to our findings (27).
Hwang et al.'s study, conducted to identify the determinants of mothers' trust in medical recommendations regarding the health of their babies, showed a significant relationship between education, income, and the race of mothers with their trust in physicians (28). These results are contrary to the findings of the current study. Freimuth et al.'s study, which examined the level of trust in African American women compared to white women, also reported a significant relationship between age, education, and income with the level of trust in white women, as well as between age and income in African American women, which differ from the results of the current study (29). Li et al.'s study contradicts the findings of the current study and shows that income, age, and settlement in a village have a significant relationship with the level of trust (30). Trust is considered a phenomenon influenced by culture, so the differences between the findings of previous studies and the current study can be largely attributed to cultural differences. The asymmetry of information between physicians and patients, especially in developing countries and particularly in centers where the vast majority of patients lack academic education (79.2%), is such that potential differences influenced by age, gender, education, and income may be overshadowed. In such societies, an intensified perception of the unquestionable scientific competence of doctors, combined with low self-confidence stemming from this information asymmetry, has created a sacred image of medical professionals. Thus, addressing the issue of trust in physicians and accurately determining its dimensions require broader mental evaluations and the use of more efficient tools. The findings of Green et al.'s study, which showed no significant relationship between family income and patients' trust in physicians, are consistent with the findings of the current study (31). The absence of a significant relationship between education and income in the present study can be interpreted primarily as a result of the high proportion of individuals with low income and education among those who visit university and government hospitals.
The difference between Zarei et al.'s study and the present study regarding the relationship between having insurance and trust in physicians can be attributed to the timing of the mentioned study (27). In 2013, the first year of implementing the health transformation plan in the country, significant financial resources were allocated to the Ministry of Health to cover the cost of inpatient treatment services and reduce out-of-pocket payments to 3-5%. Since patients attributed the incredible affordability of numerous inpatient treatment services to the efficiency of their basic or supplementary insurance coverage, this likely influenced their trust in all factors involved in the treatment process, including the doctor. Although, according to existing laws, basic insurance organizations must cover 90% of the costs of inpatient treatment services, the contribution of these organizations has been reduced for various reasons. These include indirect costs such as travel and accommodation, the prescription of drugs outside the official pharmaceutical system and outside the scope of insurance coverage, the financial inability of hospitals to purchase consumables, leading to patients being referred to buy items from the open market, and even the receipt of informal payments by a few service providers. These factors could explain the absence of a significant relationship between insurance coverage and trust in physicians in the current study. The lack of a significant relationship between having supplementary insurance and the patient's trust in the physician could be justified by the commercial nature of such insurance and its tendency to fulfill obligations minimally. Furthermore, the establishment of supplementary insurance coverage typically requires employers to conclude group contracts for employees, making it subject to the nature of these group contracts. As mentioned earlier, a large percentage of the patients in the studied hospitals represent the less privileged segments of society. Many are either unemployed and not officially affiliated with any organization capable of providing supplementary insurance contracts, or they cannot afford to pay the annual premiums for basic insurance, let alone supplementary insurance.
In the current study, the level of patient trust in the physician had a significant relationship only with the inpatient ward variable, with the trust score being higher among patients hospitalized in the internal and surgery departments compared to others. The significant correlation between the trust score and the inpatient department, as well as its higher level in the internal and surgical departments compared to burns or psychiatry, also appears reasonable, given the generally worse condition of patients in the latter departments and the extended length of their hospitalization. The relatively favorable score of patients' trust in physicians should be viewed with caution, and efforts should not be neglected to address some inherent shortcomings of the inpatient treatment service system.
Like any cross-sectional study, causal conclusions in this study should be drawn with caution. Furthermore, it is not certain that the patients' responses to the questions about trust in physicians were not influenced by their satisfaction with hospital services or their health status. Therefore, it is suggested that future studies administer the questionnaire at least one week after the patient’s discharge or include variables such as satisfaction with hospital services and general health condition at discharge in the data collection process, controlling for these variables in the analysis. In addition, as the use of questionnaires as quantitative tools for evaluating phenomena has limitations in measuring subjective variables like trust, qualitative studies should complement and enhance the depth of information obtained from these quantitative approaches. Finally, it should be noted that since the study was conducted in academic medical centers, which predominantly serve poorer and less-educated patients, caution should be exercised when generalizing the findings of this study to the broader population.
Conclusion
The slightly high overall score of the patients' trust in physicians in the two academic medical training centers under study can be explained by the composition of the patients in these hospitals, who primarily belong to lower socio-economic deciles and naturally have fewer expectations and limited awareness of their rights. Educating the public about their citizenship rights to foster public demand for addressing non-medical needs, improving the coverage of inpatient treatment costs through the quantitative and qualitative strengthening of insurance funds, reliably implementing means-tests to identify vulnerable groups and establish targeted financial support for them, and continuously enhancing the quality of physician-patient relationships with the collaboration of related organizations, particularly the medical council, are among the most critical strategies that should be considered by executive authorities in both governance and health sectors of the province.
Acknowledgement
The authors of this article acknowledge the necessity of expressing gratitude to the Vice President of Research and Technology and the Research Center for the Development of Management and Social Health of Golestan University of Medical Sciences for their cooperation in the process of reviewing and approving the project. Special thanks are also extended to the heads and managers of the Shahid Sayyad Shirazi and 5 Azar hospitals in Gorgan, as well as the nursing managers and nurses of these hospitals.
Funding sources
No Funding.
Ethical statement
This research project has been approved by the Ethics Committee of Gorgan University of Medical Sciences (IR.GOUMS.REC.1401.239).
Conflicts of interest
The authors declare no conflict of interest.
Author contributions
Abbas Badakhshan designed the study, Alireza Heidari wrote the article, Reza Mokhayyeri collected the data, and Khatirnamani performed the statistical analysis. All authors have read and approved the article.
Full-Text: (346 Views)
Introduction
Trust is an important factor in the economic and social development of communities and one of the most significant aspects of social capital (1). Mutual communications reduce the cost of economic trading and facilitate public cooperation and participation in sharing information (2,3). This issue is especially important in the health industry compared to other industries. Informational asymmetry between providers and patients, along with uncertainty in the health environment, makes the patient worry that their physician may not have adequate and up-to-date knowledge to provide the best recommendations and may impose unnecessary costs. These concerns have made the search for the best treatment a risky endeavor. A patient who visits a doctor expects that the doctor will not make their emergency a burden for profit but will make the best decision for them. This expectation is referred to as "trust" in the scientific literature. Trusting the physician is also considered an instinctive choice (4). When patients cannot independently address their health problems, they are compelled to trust the service provider (5).
Studies have shown that patients who trust their physicians more exhibit greater adherence to their treatment process (6) and are more likely to accept treatment recommendations (7). These patients will cope better if their condition becomes chronic (8). Trust in the physician is also associated with continued service from a specific provider, no delay in starting treatment, and attendance at scheduled visits (9). Although it has been stated that doctors can increase the effectiveness of treatment by using verbal and non-verbal communication skills such as respecting the patient, paying attention and empathizing with the patient, asking open questions, actively listening, and using understandable words for the patient (10), this issue has become more complicated in Iran due to inciting issues such as the use of POS machines and inducing tax evasion by physicians, highlighting and widely publishing some medical errors, falsely criminalizing some medical complications by yellow pages and elusive monitoring social media, attributing brain drain among physicians to their extravagance by some statesmen, and the struggle between the government and the medical council over the right to determine the medical tariff and bring it to the community level via media.
Different studies show varying results regarding patients' trust in their physicians and its effects. Birkhäuer et al. (8) showed a weak relationship between patients' trust and treatment outcomes, while Tran et al. (11) demonstrated the opposite. Braksmajer et al. (7) also revealed that trust in physicians had a strong association with treatment compliance. In a cohort study, Gordon et al. (12) reported that patients' trust in physicians could be strengthened through improved communication. Graham et al. (13) in their prospective study, mentioned that although there is no significant relationship between patient satisfaction with the physician and treatment outcomes, it is associated with treatment consistency.
Most of the research conducted in Iran in this field has focused on the relationship between the physician and the patient, the patient's satisfaction with the doctor, or the factors affecting trust between the doctor and the patient (14-20). A similar study with this purpose was not found in Golestan province, which is why the research team decided to design and implement this study to measure the level of patient trust in physicians in two medical teaching hospitals in Gorgan using the Wake Forest tool.
Methods
It was a cross-sectional study. The statistical population included all patients hospitalized in 5 Azar and Shaheed Sayad Shirazi educational centers affiliated with Golestan University of Medical Sciences. According to similar studies (21,22), with an SD of 6.2, a CI of 95%, and a precision of 8%, the sample size was estimated to be 243 people using the random stratified method and the following formula.
Each medical education center was considered a stratum, and the patients were randomly selected on each floor according to the number of active beds. It should be noted that in each center, sampling was done from active wards and beds where the patients were able to answer the questions and met the conditions for inclusion in the study. The inclusion criteria for the study included patients who were willing to cooperate, were over 18 years old, had been hospitalized for more than three non-holiday days, and had been visited by doctors. The exclusion criteria for the study included not being able to read, not being alert, or not being able to communicate. In addition, if the patient was not present in their bed during two visits to their bedside, they were excluded from the study. To collect data, the researcher referred to the hospital reception office and selected the desired patients according to the patient’s bed number from the table of random numbers. After attending the patient’s bedside, the patient was examined in terms of their ability to complete the questionnaire and the characteristics of withdrawal from the study. If the patient met the above-mentioned conditions, they were given explanations about the research and the questionnaire. Unconscious patients and patients in heart and brain special care units and dialysis wards were not included in this research. During the initial examination, eligible patients were assured that the resulting information would remain confidential and be used only for research purposes. Informed consent was obtained orally from the patients. To collect data, a questionnaire called the Wake Forest Questionnaire was used, which was first developed in 2002 by Hall et al. (22). Foraty Kashani et al. (23) sent the Persian translation of the questionnaire for validation by three members of the related faculty. Changes were then made to the questions based on expert opinions. A final questionnaire with 10 questions was prepared, using a 5-point Likert scale (5 = completely agree to 1 = completely disagree) to express the participants' opinions. The reliability of the questionnaire in the pilot study, based on Cronbach's alpha, was 85%. The lower, middle, and upper limits of scores are 10, 30, and 50, respectively. A score between 10 and 20 indicates low trust in the physician, 20 to 30 indicates medium trust, and above 30 indicates high trust. Data were analyzed using SPSS statistical software (Version 23, SPSS Inc., Chicago, IL). To analyze the data, descriptive statistical methods were used (e.g., drawing tables, numbers, and frequency percentages for qualitative data, and mean and standard deviation for quantitative data). In addition, due to the non-establishment of the assumption of normality of data distribution (Checked with the Kolmogorov-Smirnov test), inferential statistical methods such as Spearman correlation, Mann-Whitney, and Kruskal-Wallis tests were used. The significance level in this study was set at 0.05.
Results
The demographic and background characteristics of the 231 participants in this study are described in Table 1.
Table 2 shows the average score of the patients' trust in physicians in Shahid Sayad Shirazi and 5 Azar teaching hospitals in Gorgan. The score was 38.09±3.43 for all patients, which is evaluated as a good level.
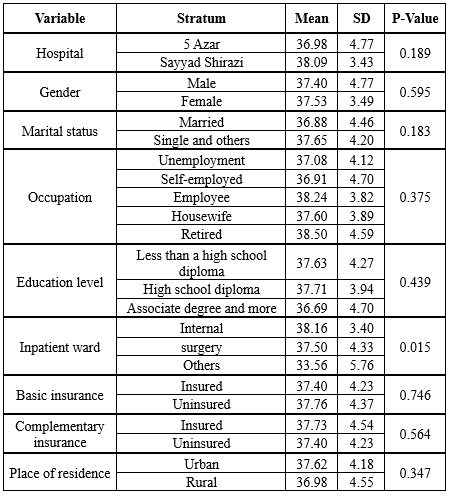
Table 3 shows the relationship between the level of the patients’ trust in physicians and demographic and contextual variables. There was a significant relationship between this level of and the inpatient ward (P-Value = 0.015); specifically, the level of trust in the internal (P-Value = 0.012) and surgery wards (P-Value = 0.041) was higher than in other wards (Burns and psychiatry). However, no statistically significant relationship was observed between other demographic and contextual variables (hospital, gender, marital status, employment status, education level, basic insurance, supplementary insurance, place of residence, age, and length of stay) and the level of the patients’ trust in physicians (P-Value > 0.05).
Trust is an important factor in the economic and social development of communities and one of the most significant aspects of social capital (1). Mutual communications reduce the cost of economic trading and facilitate public cooperation and participation in sharing information (2,3). This issue is especially important in the health industry compared to other industries. Informational asymmetry between providers and patients, along with uncertainty in the health environment, makes the patient worry that their physician may not have adequate and up-to-date knowledge to provide the best recommendations and may impose unnecessary costs. These concerns have made the search for the best treatment a risky endeavor. A patient who visits a doctor expects that the doctor will not make their emergency a burden for profit but will make the best decision for them. This expectation is referred to as "trust" in the scientific literature. Trusting the physician is also considered an instinctive choice (4). When patients cannot independently address their health problems, they are compelled to trust the service provider (5).
Studies have shown that patients who trust their physicians more exhibit greater adherence to their treatment process (6) and are more likely to accept treatment recommendations (7). These patients will cope better if their condition becomes chronic (8). Trust in the physician is also associated with continued service from a specific provider, no delay in starting treatment, and attendance at scheduled visits (9). Although it has been stated that doctors can increase the effectiveness of treatment by using verbal and non-verbal communication skills such as respecting the patient, paying attention and empathizing with the patient, asking open questions, actively listening, and using understandable words for the patient (10), this issue has become more complicated in Iran due to inciting issues such as the use of POS machines and inducing tax evasion by physicians, highlighting and widely publishing some medical errors, falsely criminalizing some medical complications by yellow pages and elusive monitoring social media, attributing brain drain among physicians to their extravagance by some statesmen, and the struggle between the government and the medical council over the right to determine the medical tariff and bring it to the community level via media.
Different studies show varying results regarding patients' trust in their physicians and its effects. Birkhäuer et al. (8) showed a weak relationship between patients' trust and treatment outcomes, while Tran et al. (11) demonstrated the opposite. Braksmajer et al. (7) also revealed that trust in physicians had a strong association with treatment compliance. In a cohort study, Gordon et al. (12) reported that patients' trust in physicians could be strengthened through improved communication. Graham et al. (13) in their prospective study, mentioned that although there is no significant relationship between patient satisfaction with the physician and treatment outcomes, it is associated with treatment consistency.
Most of the research conducted in Iran in this field has focused on the relationship between the physician and the patient, the patient's satisfaction with the doctor, or the factors affecting trust between the doctor and the patient (14-20). A similar study with this purpose was not found in Golestan province, which is why the research team decided to design and implement this study to measure the level of patient trust in physicians in two medical teaching hospitals in Gorgan using the Wake Forest tool.
Methods
It was a cross-sectional study. The statistical population included all patients hospitalized in 5 Azar and Shaheed Sayad Shirazi educational centers affiliated with Golestan University of Medical Sciences. According to similar studies (21,22), with an SD of 6.2, a CI of 95%, and a precision of 8%, the sample size was estimated to be 243 people using the random stratified method and the following formula.
Each medical education center was considered a stratum, and the patients were randomly selected on each floor according to the number of active beds. It should be noted that in each center, sampling was done from active wards and beds where the patients were able to answer the questions and met the conditions for inclusion in the study. The inclusion criteria for the study included patients who were willing to cooperate, were over 18 years old, had been hospitalized for more than three non-holiday days, and had been visited by doctors. The exclusion criteria for the study included not being able to read, not being alert, or not being able to communicate. In addition, if the patient was not present in their bed during two visits to their bedside, they were excluded from the study. To collect data, the researcher referred to the hospital reception office and selected the desired patients according to the patient’s bed number from the table of random numbers. After attending the patient’s bedside, the patient was examined in terms of their ability to complete the questionnaire and the characteristics of withdrawal from the study. If the patient met the above-mentioned conditions, they were given explanations about the research and the questionnaire. Unconscious patients and patients in heart and brain special care units and dialysis wards were not included in this research. During the initial examination, eligible patients were assured that the resulting information would remain confidential and be used only for research purposes. Informed consent was obtained orally from the patients. To collect data, a questionnaire called the Wake Forest Questionnaire was used, which was first developed in 2002 by Hall et al. (22). Foraty Kashani et al. (23) sent the Persian translation of the questionnaire for validation by three members of the related faculty. Changes were then made to the questions based on expert opinions. A final questionnaire with 10 questions was prepared, using a 5-point Likert scale (5 = completely agree to 1 = completely disagree) to express the participants' opinions. The reliability of the questionnaire in the pilot study, based on Cronbach's alpha, was 85%. The lower, middle, and upper limits of scores are 10, 30, and 50, respectively. A score between 10 and 20 indicates low trust in the physician, 20 to 30 indicates medium trust, and above 30 indicates high trust. Data were analyzed using SPSS statistical software (Version 23, SPSS Inc., Chicago, IL). To analyze the data, descriptive statistical methods were used (e.g., drawing tables, numbers, and frequency percentages for qualitative data, and mean and standard deviation for quantitative data). In addition, due to the non-establishment of the assumption of normality of data distribution (Checked with the Kolmogorov-Smirnov test), inferential statistical methods such as Spearman correlation, Mann-Whitney, and Kruskal-Wallis tests were used. The significance level in this study was set at 0.05.
Results
The demographic and background characteristics of the 231 participants in this study are described in Table 1.
Table 2 shows the average score of the patients' trust in physicians in Shahid Sayad Shirazi and 5 Azar teaching hospitals in Gorgan. The score was 38.09±3.43 for all patients, which is evaluated as a good level.
Table 3 shows the relationship between the level of the patients’ trust in physicians and demographic and contextual variables. There was a significant relationship between this level of and the inpatient ward (P-Value = 0.015); specifically, the level of trust in the internal (P-Value = 0.012) and surgery wards (P-Value = 0.041) was higher than in other wards (Burns and psychiatry). However, no statistically significant relationship was observed between other demographic and contextual variables (hospital, gender, marital status, employment status, education level, basic insurance, supplementary insurance, place of residence, age, and length of stay) and the level of the patients’ trust in physicians (P-Value > 0.05).
|
Table 1. The demographic and background characteristics of the study participants
 |
|
Table 2. The average score of the patient's trust in the physician in the educational hospitals of Gorgan
 |
|
Table 3. Correlation between the patients’ level of trust in the physicians with demographic and contextual variables
 |
Discussion
Based on the present study, the patients’ trust in physicians in both Sayyad Shirazi and 5 Azar Gorgan hospitals was determined to be at an optimal level. This rate was lower compared to the studies of Hall et al. (22) and Foraty et al. (24). Even though the result may be due to the high trust of the patients in physicians as a result of appropriate medical services and the high skill of physicians, patients admitted to medical teaching hospitals mostly include individuals with lower financial ability who may have lower expectations of medical services and higher trust in physicians. It seems that the expenses incurred in recent years, resulting from spending the funds of the Health Transformation Plan to purchase advanced medical equipment, renovate and improve the physical space of hospitals, and enhance care due to the increase in nursing manpower during the peak of the COVID-19 pandemic, are a confounding factor in measuring patients' trust in physicians. It should also be kept in mind that, despite emphasizing the confidentiality of the questionnaire information and its lack of impact on the treatment process, some patients may not have answered honestly.
The absence of a significant relationship between the trust score and background and demographic variables in the present study is largely consistent with the findings of Graham et al.'s study. In their study, there was no significant relationship between gender, race, and education with trust in the physician. The findings of Englehart et al.'s study, mentioning no significant relationship between demographic variables such as age, marital status, and education level with their level of trust, are consistent with the findings of the current study (25). The findings of Kim et al.'s study are in some respects consistent with the findings of the current study. In the mentioned study, no significant relationship was found between age, education, place of residence, type of insurance, and home ownership with trust in the physician. However, the study showed a significant relationship between the variables of income and gender and the level of trust in the physician, such that as income decreased, the level of trust in the physician also decreased, and female patients had 0.67 less trust in physicians than men (26). Zarei et al. observed no significant relationship between patients' trust in physicians and variables such as age, sex, and education, which is in accordance with the results of the current study. However, findings such as a significant relationship between covered insurance and trust in physicians are contrary to our findings (27).
Hwang et al.'s study, conducted to identify the determinants of mothers' trust in medical recommendations regarding the health of their babies, showed a significant relationship between education, income, and the race of mothers with their trust in physicians (28). These results are contrary to the findings of the current study. Freimuth et al.'s study, which examined the level of trust in African American women compared to white women, also reported a significant relationship between age, education, and income with the level of trust in white women, as well as between age and income in African American women, which differ from the results of the current study (29). Li et al.'s study contradicts the findings of the current study and shows that income, age, and settlement in a village have a significant relationship with the level of trust (30). Trust is considered a phenomenon influenced by culture, so the differences between the findings of previous studies and the current study can be largely attributed to cultural differences. The asymmetry of information between physicians and patients, especially in developing countries and particularly in centers where the vast majority of patients lack academic education (79.2%), is such that potential differences influenced by age, gender, education, and income may be overshadowed. In such societies, an intensified perception of the unquestionable scientific competence of doctors, combined with low self-confidence stemming from this information asymmetry, has created a sacred image of medical professionals. Thus, addressing the issue of trust in physicians and accurately determining its dimensions require broader mental evaluations and the use of more efficient tools. The findings of Green et al.'s study, which showed no significant relationship between family income and patients' trust in physicians, are consistent with the findings of the current study (31). The absence of a significant relationship between education and income in the present study can be interpreted primarily as a result of the high proportion of individuals with low income and education among those who visit university and government hospitals.
The difference between Zarei et al.'s study and the present study regarding the relationship between having insurance and trust in physicians can be attributed to the timing of the mentioned study (27). In 2013, the first year of implementing the health transformation plan in the country, significant financial resources were allocated to the Ministry of Health to cover the cost of inpatient treatment services and reduce out-of-pocket payments to 3-5%. Since patients attributed the incredible affordability of numerous inpatient treatment services to the efficiency of their basic or supplementary insurance coverage, this likely influenced their trust in all factors involved in the treatment process, including the doctor. Although, according to existing laws, basic insurance organizations must cover 90% of the costs of inpatient treatment services, the contribution of these organizations has been reduced for various reasons. These include indirect costs such as travel and accommodation, the prescription of drugs outside the official pharmaceutical system and outside the scope of insurance coverage, the financial inability of hospitals to purchase consumables, leading to patients being referred to buy items from the open market, and even the receipt of informal payments by a few service providers. These factors could explain the absence of a significant relationship between insurance coverage and trust in physicians in the current study. The lack of a significant relationship between having supplementary insurance and the patient's trust in the physician could be justified by the commercial nature of such insurance and its tendency to fulfill obligations minimally. Furthermore, the establishment of supplementary insurance coverage typically requires employers to conclude group contracts for employees, making it subject to the nature of these group contracts. As mentioned earlier, a large percentage of the patients in the studied hospitals represent the less privileged segments of society. Many are either unemployed and not officially affiliated with any organization capable of providing supplementary insurance contracts, or they cannot afford to pay the annual premiums for basic insurance, let alone supplementary insurance.
In the current study, the level of patient trust in the physician had a significant relationship only with the inpatient ward variable, with the trust score being higher among patients hospitalized in the internal and surgery departments compared to others. The significant correlation between the trust score and the inpatient department, as well as its higher level in the internal and surgical departments compared to burns or psychiatry, also appears reasonable, given the generally worse condition of patients in the latter departments and the extended length of their hospitalization. The relatively favorable score of patients' trust in physicians should be viewed with caution, and efforts should not be neglected to address some inherent shortcomings of the inpatient treatment service system.
Like any cross-sectional study, causal conclusions in this study should be drawn with caution. Furthermore, it is not certain that the patients' responses to the questions about trust in physicians were not influenced by their satisfaction with hospital services or their health status. Therefore, it is suggested that future studies administer the questionnaire at least one week after the patient’s discharge or include variables such as satisfaction with hospital services and general health condition at discharge in the data collection process, controlling for these variables in the analysis. In addition, as the use of questionnaires as quantitative tools for evaluating phenomena has limitations in measuring subjective variables like trust, qualitative studies should complement and enhance the depth of information obtained from these quantitative approaches. Finally, it should be noted that since the study was conducted in academic medical centers, which predominantly serve poorer and less-educated patients, caution should be exercised when generalizing the findings of this study to the broader population.
Conclusion
The slightly high overall score of the patients' trust in physicians in the two academic medical training centers under study can be explained by the composition of the patients in these hospitals, who primarily belong to lower socio-economic deciles and naturally have fewer expectations and limited awareness of their rights. Educating the public about their citizenship rights to foster public demand for addressing non-medical needs, improving the coverage of inpatient treatment costs through the quantitative and qualitative strengthening of insurance funds, reliably implementing means-tests to identify vulnerable groups and establish targeted financial support for them, and continuously enhancing the quality of physician-patient relationships with the collaboration of related organizations, particularly the medical council, are among the most critical strategies that should be considered by executive authorities in both governance and health sectors of the province.
Acknowledgement
The authors of this article acknowledge the necessity of expressing gratitude to the Vice President of Research and Technology and the Research Center for the Development of Management and Social Health of Golestan University of Medical Sciences for their cooperation in the process of reviewing and approving the project. Special thanks are also extended to the heads and managers of the Shahid Sayyad Shirazi and 5 Azar hospitals in Gorgan, as well as the nursing managers and nurses of these hospitals.
Funding sources
No Funding.
Ethical statement
This research project has been approved by the Ethics Committee of Gorgan University of Medical Sciences (IR.GOUMS.REC.1401.239).
Conflicts of interest
The authors declare no conflict of interest.
Author contributions
Abbas Badakhshan designed the study, Alireza Heidari wrote the article, Reza Mokhayyeri collected the data, and Khatirnamani performed the statistical analysis. All authors have read and approved the article.
Type of Study: Original Article |
Subject:
Health economic
Received: 2024/11/20 | Accepted: 2024/12/10
Received: 2024/11/20 | Accepted: 2024/12/10
References
1. Moidfar S, Jahangiri P. Generalized social trust and social factors affecting: A case study in Urmia. Journal of Historical Sociology. 2009;1(1):47-67. [View at Publisher] [Google Scholar]
2. Dearmon J, Grier K. Trust and development. Journal of Economic Behavior & Organization. 2009;71(2):210-20. [View at Publisher] [DOI] [Google Scholar]
3. Durlauf SN. On the empirics of social capital. The economic journal. 2002;112(483):F459-79. [View at Publisher] [DOI] [Google Scholar]
4. Egede LE, Ellis C. Development and Testing of the Multidimensional Trust in Health Care Systems Scale. J Gen Intern Med. 2008;23(6):808-15. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Hillen MA, De Haes HC, Smets EM. Cancer patients' trust in their physician-a review. Psychooncology. 2011;20(3):227-41. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Becker ER, Roblin DW. Translating Primary Care Practice Climate into Patient Activation: The Role of Patient Trust in Physician. Medical Care. 2008;46(8):795-805. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Braksmajer A, Fedor TM, Chen S-R, Corales R, Holt S, Valenti W, et al. Willingness to take PrEP for HIV prevention: The combined effects of race/ethnicity and provider trust. AIDS Education and Prevention. 2018;30(1):1-12. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Birkhäuer J, Gaab J, Kossowsky J, Hasler S, Krummenacher P, Werner C, et al. Trust in the health care professional and health outcome: A meta-analysis. PloS One. 2017;12(2):e0170988. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Hillen MA, Butow PN, Tattersall MHN, Hruby G, Boyle FM, Vardy J, et al. Validation of the English version of the Trust in Oncologist Scale (TiOS). Patient Educ Couns. 2013;91(1):25-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Roh H, Park KH, Park SY. Verbal communication of students with high patient-physician interaction scores in a clinical performance examination assessed by standardized patients. Korean J Med Educ. 2017;29(4):241-51. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Tran DQ, Barry V, Antun A, Ribeiro M, Stein S, Kempton CL. Physician trust and depression influence adherence to factor replacement: a single‐centre cross‐sectional study. Haemophilia. 2017;23(1):98-104. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Gordon HS, Pugach O, Berbaum ML, Ford ME. Examining patients' trust in physicians and the VA healthcare system in a prospective cohort followed for six-months after an exacerbation of heart failure. Patient Educ Couns. 2014;97(2):173-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Graham JL, Shahani L, Grimes RM, Hartman C, Giordano TP. The influence of trust in physicians and trust in the healthcare system on linkage, retention, and adherence to HIV care. AIDS Patient Care STDS. 2015;29(12):661-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Movahed M, Salehi A, Rayanpour R. Quality of Doctor-Patient Relationship and its Effect on Usage of Traditional and Complementary Medicine. Journal of Isfahan Medical School. 2017;35(421):177-85. [View at Publisher] [Google Scholar]
15. Shafati M, Zahedi MJ. Physician-patient relationship: ethnography of multiple patient visits at private offices of doctors. 2014;2(1):46-61. [View at Publisher] [Google Scholar]
16. Zahednezhad H, Poursharifi Ha, Babapour J. Relationship betweeh health locus of control, slip memory and physician-patient relationship with adherence in Type II diabetic patients. J Shahid Sadoughi Univ Med Sci. 2012;20(2):249-58. [View at Publisher] [Google Scholar]
17. Bastani P, Hashemi N, Bahrami MA. Correlation of patients' health literacy and physician-patient interaction: A case study in Shahid Faghihi hospital, Shiraz, 2019. Management Strategies in Health System. 2019;4(1):47-56. [View at Publisher] [DOI] [Google Scholar]
18. Banidavoodi S, Hoseizadeh M, Maraghi E. Assessment of physicians' communication with patients in Ahvaz Hospitals from Patient and observer'Perspectives. Educational Development of Judishapur. 2013;4(4):65-71. [View at Publisher] [Google Scholar]
19. Amerion A, Karimi Zarchi A, Tofighi Sh, Zaboli R, Rafati H. Inpatient and outpatient satisfaction of a military hospital. J Mil Med. 2009;11(1):37-44. [View at Publisher] [Google Scholar]
20. Narenjiha M HS, Baahador H, Shajari J, Haji Molla Hoseini F. The effect of physicians' communication skills on patients' satisfaction. Iranian Journal of Medical Education. 2012;12(1):77-89. [View at Publisher] [DOI] [Google Scholar]
21. Khammarnia M, Hashemi Karghash Z, Peyvand M, Ramezani F. A Survey on Trust to Hospital Services after Health Transformation Plan. Payesh (Health Monitor). 2020;19(3):243-54. [View at Publisher] [DOI] [Google Scholar]
22. Hall MA, Zheng B, Dugan E, Camacho F, Kidd KE, Mishra A, et al. Measuring patients' trust in their primary care providers. Med Care Res Rev. 2002;59(3):293-318. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Foraty Kashani M, Dabiran S, M Noroozi. Examining the professional commitment of specialized assistants of Tehran University of Medical Sciences from the perspective of patients. Iranian Journal of Medical Ethics and History of Medicine. 2010;3(4):46-56. [View at Publisher]
24. Foraty H, Esparham R, Dargahi M. Assessing and Prioritizing the Factors Affecting the Patient's Trust in the Physician from the Point of View of Experts in Ilam University of Medical Sciences in 2018 with the Combined Approach of DEMATEL and ANP. Alborz Univ Med J. 2020;9(1 ):9-20. [View at Publisher] [DOI] [Google Scholar]
25. Engelhardt EG, Smets EM, Sorial I, Stiggelbout AM, Pieterse AH, Hillen MA. Is there a relationship between shared decision making and breast cancer patients' trust in their medical oncologists? Med Decis Making. 2020;40(1):52-61. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Kim-Soon N. Entrepreneurial Motivation and Entreprenuership Intention Published IBIMA Milan Italy. 2014. p.1001-1011. [View at Publisher]
27. Zarei E, Daneshkohan A, Khabiri R, Arab M. The effect of hospital service quality on patient's trust. Iran Red Crescent Med J. 2014;17(1):e17505. [View at Publisher] [DOI] [PMID] [Google Scholar]
28. Hwang SS, Rybin DV, Kerr SM, Heeren TC, Colson ER, Corwin MJ. Predictors of Maternal Trust in Doctors About Advice on Infant Care Practices: The SAFE Study. Acad Pediatr. 2017;17(7):762-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
29. Freimuth VS, Jamison AM, An J, Hancock GR, Quinn SC. Determinants of trust in the flu vaccine for African Americans and Whites. Soc Sci Med. 2017;193:70-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
30. Li YB, James L, McKibben J. Trust between physicians and patients in the e-health era. Technology in Society. 2016;46:28-34. [View at Publisher] [DOI] [Google Scholar]
31. Greene J, Ramos C. A mixed methods examination of health care provider behaviors that build patients' trust. Patient Educ Couns. 2021;104(5):1222-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |