Mon, Feb 9, 2026
[Archive]
Efficacy of diabetes nutrition counseling on metabolic factors and knowledge, attitude, and practice
Amirhossein Gholamnia Khatir1 

 , Ali Jafari2
, Ali Jafari2 

 , Atena Mohammadian1
, Atena Mohammadian1 

 , Javad Heshmati3
, Javad Heshmati3 

 , Motahareh Hasani *4
, Motahareh Hasani *4 




 , Ali Jafari2
, Ali Jafari2 

 , Atena Mohammadian1
, Atena Mohammadian1 

 , Javad Heshmati3
, Javad Heshmati3 

 , Motahareh Hasani *4
, Motahareh Hasani *4 


1- School of Medicine, Golestan University of Medical Sciences and Health Services, Gorgan, Iran
2- Department of Community Nutrition, School of Nutrition Sciences and Food Technology, Shahid Beheshti University of Medical Sciences, Tehran, Iran
3- Department of Public Health, Songhor Healthcare Center, Kermanshah University of Medical Sciences, Kermanshah, Iran
4- Department of Nutritional Sciences, School of Health, Golestan University of Medical Sciences, Gorgan, Iran; Metabolic Disorders Research Center, Golestan University of Medical Sciences, Gorgan, Iran
2- Department of Community Nutrition, School of Nutrition Sciences and Food Technology, Shahid Beheshti University of Medical Sciences, Tehran, Iran
3- Department of Public Health, Songhor Healthcare Center, Kermanshah University of Medical Sciences, Kermanshah, Iran
4- Department of Nutritional Sciences, School of Health, Golestan University of Medical Sciences, Gorgan, Iran; Metabolic Disorders Research Center, Golestan University of Medical Sciences, Gorgan, Iran
Keywords: Knowledge, Attitude, Professional Practice, Diabetes Mellitus, Type 2, Diet, Food, and Nutrition
Full-Text [PDF 388 kb]
(340 Downloads)
| Abstract (HTML) (2368 Views)
Discussion
The current study aimed to investigate the effectiveness of nutrition experts' presence on various biochemical parameters, including blood sugar, BMI, awareness, attitude, and practice in patients with type 2 diabetes. The study's results demonstrated that nutrition education provided to the patients led to the control of fasting blood sugar and glycosylated hemoglobin levels. These findings are consistent with previous studies by Sharifi Rad et al. (15) and Kashfi et al. (16), which reported significant reductions in fasting blood sugar levels after nutrition education interventions.
The study did not find a significant difference between the exposure and non-exposure groups regarding BMI as an anthropometric index. This aligns with the findings of Maheri et al. (17), who also observed no significant difference in BMI between the exposure and non-exposure groups in their study. Similarly, there were no significant changes in average weight and waist circumference before and after the educational intervention. However, HbA1c and fasting blood sugar levels significantly decreased in the intervention group, which is consistent with the present study.
Numerous studies have demonstrated the effectiveness of educational interventions in improving the nutritional status of diabetic patients. Studies by Heydari et al. (18) and Gucciardi et al. (19) have shown positive impacts of educational interventions on the nutritional performance of diabetic patients. Thus, educating diabetic patients about proper nutrition and ensuring follow-up can improve their nutritional status.
Considering the importance of a proper diet for type 2 diabetic patients, it is recommended that training courses be organized in healthcare centers and other diabetes-related organizations. Regular training courses conducted by official bodies can yield better results due to the availability of appropriate educational facilities and qualified experts. The significance of continuous education should not be overlooked, as demonstrated by the study conducted at the Yazd Diabetes Center by Baghian Moghadam (20) which showed a significant reduction in HbA1c levels after a five-month educational intervention.
It is important to note that raising awareness about the importance of food and nutrition education alone is not sufficient for diabetes control. Strategies should be implemented to enhance patients' awareness, attitude, and practice. In the present study, there was no significant difference in the knowledge, attitude, and practice scores between the exposure and non-exposure groups. One reason for the decline in scores in the exposure group was the limited utilization of the meal plans provided by the nutritionist. Additionally, the non-exposure group engaged in personal participation in classes, workshops, and media and virtual training, which were not recorded and evaluated. The findings of Mandana Goodarzi et al. (21) on the relationship between knowledge, attitude, practice, and self-efficacy of type 2 diabetic patients somewhat align with the present study's findings.
In summary, the study highlights the effectiveness of nutrition education in controlling blood sugar levels and glycosylated hemoglobin in patients with type 2 diabetes. While no significant changes were observed in BMI, continuous education and comprehensive approaches to improving patients' knowledge, attitude, and practice should be emphasized. Regular training courses by official bodies can play a vital role in enhancing the nutritional status and overall well-being of diabetic patients.
Conclusion
This study's findings demonstrate the effectiveness of educational interventions in reducing fasting blood sugar and HbA1c levels among type 2 diabetic patients in the exposure group compared to the non-exposure group. These results indicate the positive impact of diet and physical activity education on diabetes management. However, further clinical trials are needed to draw more robust conclusions. It is important to note that while other studies have shown improvements in awareness, attitude, and practice, this study did not find significant changes in these scores. Therefore, it is recommended that control, monitoring, and educational follow-up measures be implemented in similar programs.
The outcomes of this research provide a foundation for future studies, including the design and evaluation of educational-supportive interventions.
Acknowledgement
The authors express their gratitude to Golestan University of Medical Sciences for their assistance in recruiting patients for this study.
Funding sources
Golestan University of Medical Sciences approved and funded this research under grant number 113268.
Ethical statement
Approval from the Ethics Committee of Golestan University of Medical Sciences (IR.GOUMS.REC.1401.510) was obtained prior to conducting the study. Consent for participation was obtained from the patients through an opt-out document, ensuring their voluntary involvement.
Conflicts of interest
The authors declare no conflicts of interest associated with this research.
Author contributions
Conceptualization, AGh and MH; methodology, MH; validation, AGh and AM; investigation, AGh and AJ; resources, AGh and JH; data curation, MH and JH; writing-original draft preparation, AGh and AJ; writing-review and editing, MH; visualization, MH; supervision, MH; project administration, MH. All authors have read and agreed to the published version of the manuscript.
Full-Text: (366 Views)
Introduction
Diabetes has become a rapidly growing global health concern, with projections indicating that it will affect approximately 693 million adults by 2045 (1). Specifically, the incidence of type 2 diabetes has been steadily increasing, contributing significantly to this rise (2). To mitigate the complications associated with diabetes, management strategies often emphasize lifestyle modifications, such as increased physical activity and dietary interventions (3). Among healthcare professionals, nurses, experts, and paramedics play a pivotal role in monitoring, educating, and supporting individuals with diabetes and their families (4). Nutritional therapy is a vital and fundamental component of treatment, necessitating evidence-based recommendations and consideration of potential drug interactions (5). Numerous randomized trials, meta-analyses, and case studies have demonstrated the beneficial outcomes of low-carbohydrate diets in treating diabetes, prediabetes, metabolic syndrome, and obesity (6). Successful implementation of this diet has been associated with improvements in weight loss, reduced medication dosages, and even the reversal of type 2 diabetes in some cases (6).
Cardiovascular diseases represent the most prevalent complications associated with type 2 diabetes and remain the leading cause of mortality within this population and beyond. Emerging data support the influence of nutritional factors not only on achieving metabolic targets in diabetes but also on cardiovascular risk factors (7). The Academy of Nutrition and Dietetics highlights the effectiveness of nutrition therapy registered dietitians provide for adults with prediabetes or type 2 diabetes, as it leads to improved medical outcomes and enhanced quality of life. Consequently, integrating nutrition and therapeutic programs into healthcare systems and public health initiatives, along with appropriate reimbursement, becomes imperative (8).
Medical nutrition therapy constitutes a key pillar in diabetes management, emphasizing the importance of macronutrient balance, carbohydrate load reduction, glycemic index control, and adopting a healthy eating pattern (9). Accurate nutrition assessment using suitable tools and balanced and regularly supervised physical activity contribute to developing effective care plans tailored to the specific needs of older individuals with diabetes (10). Nutritional interventions for diabetes management may involve calorie reduction, the adoption of low glycemic index diets, and increased dietary fiber content (11). While prior research has highlighted the effectiveness of nutrition care registered dietitians provide in primary healthcare settings, comprehensive reviews in this area remain lacking (12). Future investigations may explore novel approaches to nutrition counseling within multidisciplinary teams to more effectively address cardiovascular risk factors (12).
The present study aims to investigate the effectiveness of having a nutrition expert in health centers located in our city, focusing on patients aged 30 years and above with type 2 diabetes registered in the registry system. Given the decreased quality of life experienced by patients, the challenges related to dietary restrictions, weight control, medication adherence, and continuous blood sugar monitoring, as well as the physical, mental, and social complications associated with diabetes, it is important to ascertain the potential impact of educational and emotional support services. Specifically, we seek to determine how the presence of a nutrition expert and the services they provide to diabetic patients can contribute to improvements in blood sugar control indicators, anthropometric indices, awareness, attitudes, and practices related to diabetes management.
Methods
Study design and participant selection
This retrospective cohort study involved 156 type 2 diabetes patients. The study protocol was approved by our university's ethics committee, and all participants provided their written informed consent.
The inclusion criteria for the study were: a) age 30-80 years, b) type 2 diabetes patients registered in the lean system, c) use of oral medications or insulin for blood sugar control, d) regular visits (At least once) to the centers, e) at least six months since the last course attended, f) a complete medical record and participation in nutrition education programs in the centers, g) laboratory information recorded during referrals, and h) participation in at least one of the training courses. The exclusion criteria included the presence of underlying diseases, such as kidney disease and heart disease. We included 78 participants from the group that received nutrition education from a nutritionist tailored to type 2 diabetes and 78 participants from the group that did not receive such education. We calculated the sample size for this research based on a power of 0.9 and a confidence level of 95% to estimate the mean difference in HbA1c and FBS (13).
The participants were selected using a simple random method from the registry of type 2 diabetes patients in the local health system of Golestan University of Medical Sciences, located in northeast Iran.
Data collection
We obtained data on the participants’ demographic characteristics and potential confounders from the registry system. Data was collected using a four-section questionnaire covering personal-social characteristics, knowledge, attitude, and practice. Each section contained 10 questions. The questionnaire, developed by Mehtab Niromand et al. in 2016, was tested for reliability and validity, with Cronbach’s alpha values of at least 0.75 in each section (14).
After recording the necessary information, phone calls were made to the participants to complete the questionnaires. To ensure unbiased responses and avoid the researcher's influence, the phone calls were conducted anonymously, without disclosing information about the participants' group assignment, level of education, knowledge, or other variables.
Lack of access to and incompleteness of many patients' records caused many participants to leave the study and affected the sample size of the present study.
Data analysis
The Statistical Package for the Social Sciences (SPSS, version 22.0) was used for data analysis. Mean ± SD for numerical data and frequencies for categorical data were used to present the findings. The Chi-square test was used to test the association between proportions. The independent t-test was used to compare the means of variables between the two groups under normal conditions. The Mann-Whitney test was employed for non-normally distributed variables. A significance level of less than 0.05 was considered statistically significant.
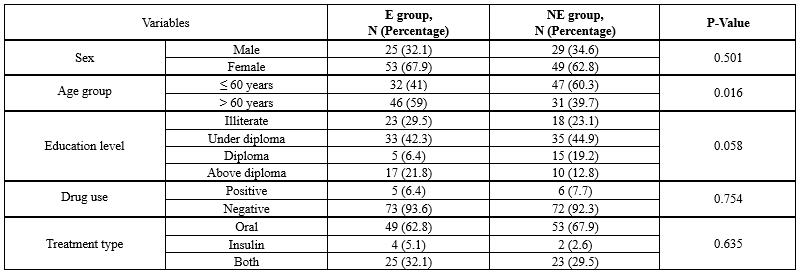
Results
The participants included 54 men and 102 women aged 30 to 80. Most participants had an education below a diploma, and only 17.3% had a university education. More than 30% of patients controlled their diabetes using insulin, while the others used oral drugs. The exposure and non-exposure groups were comparable regarding their baseline characteristics, as statistical tests detected no significant differences. The demographic information of the participants in the study, separated by exposure and non-exposure groups, is shown in Table 1.
Table 2 describes the average body mass index (BMI), fasting blood sugar, and HbA1C in the exposure group, which were 28.09 ± 5.01, 147.76 ± 50.09, and 7.25 ± 1.44, respectively. In the non-exposure group, these values were 29.45 ± 4.26, 173.24 ± 71.57, and 8.30 ± 1.92, respectively. There was no significant difference in the average BMI between the two groups, but a significant difference was observed in the other two parameters.
Additionally, as observed in Table 2, scores for the knowledge, attitude, and practice of participants in the questionnaire were recorded. The average knowledge, attitude, and practice scores in the exposure group were 55.54 ± 13.99, 26.15 ± 14.03, and 41.92 ± 14.69, respectively. These scores in the non-exposure group were 52.56 ± 13.24, 26.01 ± 14.85, and 41.47 ± 15.02, respectively. Although the scores were higher in the exposure group, no statistically significant differences existed in any of the categories.
Diabetes has become a rapidly growing global health concern, with projections indicating that it will affect approximately 693 million adults by 2045 (1). Specifically, the incidence of type 2 diabetes has been steadily increasing, contributing significantly to this rise (2). To mitigate the complications associated with diabetes, management strategies often emphasize lifestyle modifications, such as increased physical activity and dietary interventions (3). Among healthcare professionals, nurses, experts, and paramedics play a pivotal role in monitoring, educating, and supporting individuals with diabetes and their families (4). Nutritional therapy is a vital and fundamental component of treatment, necessitating evidence-based recommendations and consideration of potential drug interactions (5). Numerous randomized trials, meta-analyses, and case studies have demonstrated the beneficial outcomes of low-carbohydrate diets in treating diabetes, prediabetes, metabolic syndrome, and obesity (6). Successful implementation of this diet has been associated with improvements in weight loss, reduced medication dosages, and even the reversal of type 2 diabetes in some cases (6).
Cardiovascular diseases represent the most prevalent complications associated with type 2 diabetes and remain the leading cause of mortality within this population and beyond. Emerging data support the influence of nutritional factors not only on achieving metabolic targets in diabetes but also on cardiovascular risk factors (7). The Academy of Nutrition and Dietetics highlights the effectiveness of nutrition therapy registered dietitians provide for adults with prediabetes or type 2 diabetes, as it leads to improved medical outcomes and enhanced quality of life. Consequently, integrating nutrition and therapeutic programs into healthcare systems and public health initiatives, along with appropriate reimbursement, becomes imperative (8).
Medical nutrition therapy constitutes a key pillar in diabetes management, emphasizing the importance of macronutrient balance, carbohydrate load reduction, glycemic index control, and adopting a healthy eating pattern (9). Accurate nutrition assessment using suitable tools and balanced and regularly supervised physical activity contribute to developing effective care plans tailored to the specific needs of older individuals with diabetes (10). Nutritional interventions for diabetes management may involve calorie reduction, the adoption of low glycemic index diets, and increased dietary fiber content (11). While prior research has highlighted the effectiveness of nutrition care registered dietitians provide in primary healthcare settings, comprehensive reviews in this area remain lacking (12). Future investigations may explore novel approaches to nutrition counseling within multidisciplinary teams to more effectively address cardiovascular risk factors (12).
The present study aims to investigate the effectiveness of having a nutrition expert in health centers located in our city, focusing on patients aged 30 years and above with type 2 diabetes registered in the registry system. Given the decreased quality of life experienced by patients, the challenges related to dietary restrictions, weight control, medication adherence, and continuous blood sugar monitoring, as well as the physical, mental, and social complications associated with diabetes, it is important to ascertain the potential impact of educational and emotional support services. Specifically, we seek to determine how the presence of a nutrition expert and the services they provide to diabetic patients can contribute to improvements in blood sugar control indicators, anthropometric indices, awareness, attitudes, and practices related to diabetes management.
Methods
Study design and participant selection
This retrospective cohort study involved 156 type 2 diabetes patients. The study protocol was approved by our university's ethics committee, and all participants provided their written informed consent.
The inclusion criteria for the study were: a) age 30-80 years, b) type 2 diabetes patients registered in the lean system, c) use of oral medications or insulin for blood sugar control, d) regular visits (At least once) to the centers, e) at least six months since the last course attended, f) a complete medical record and participation in nutrition education programs in the centers, g) laboratory information recorded during referrals, and h) participation in at least one of the training courses. The exclusion criteria included the presence of underlying diseases, such as kidney disease and heart disease. We included 78 participants from the group that received nutrition education from a nutritionist tailored to type 2 diabetes and 78 participants from the group that did not receive such education. We calculated the sample size for this research based on a power of 0.9 and a confidence level of 95% to estimate the mean difference in HbA1c and FBS (13).
The participants were selected using a simple random method from the registry of type 2 diabetes patients in the local health system of Golestan University of Medical Sciences, located in northeast Iran.
Data collection
We obtained data on the participants’ demographic characteristics and potential confounders from the registry system. Data was collected using a four-section questionnaire covering personal-social characteristics, knowledge, attitude, and practice. Each section contained 10 questions. The questionnaire, developed by Mehtab Niromand et al. in 2016, was tested for reliability and validity, with Cronbach’s alpha values of at least 0.75 in each section (14).
After recording the necessary information, phone calls were made to the participants to complete the questionnaires. To ensure unbiased responses and avoid the researcher's influence, the phone calls were conducted anonymously, without disclosing information about the participants' group assignment, level of education, knowledge, or other variables.
Lack of access to and incompleteness of many patients' records caused many participants to leave the study and affected the sample size of the present study.
Data analysis
The Statistical Package for the Social Sciences (SPSS, version 22.0) was used for data analysis. Mean ± SD for numerical data and frequencies for categorical data were used to present the findings. The Chi-square test was used to test the association between proportions. The independent t-test was used to compare the means of variables between the two groups under normal conditions. The Mann-Whitney test was employed for non-normally distributed variables. A significance level of less than 0.05 was considered statistically significant.
Results
The participants included 54 men and 102 women aged 30 to 80. Most participants had an education below a diploma, and only 17.3% had a university education. More than 30% of patients controlled their diabetes using insulin, while the others used oral drugs. The exposure and non-exposure groups were comparable regarding their baseline characteristics, as statistical tests detected no significant differences. The demographic information of the participants in the study, separated by exposure and non-exposure groups, is shown in Table 1.
Table 2 describes the average body mass index (BMI), fasting blood sugar, and HbA1C in the exposure group, which were 28.09 ± 5.01, 147.76 ± 50.09, and 7.25 ± 1.44, respectively. In the non-exposure group, these values were 29.45 ± 4.26, 173.24 ± 71.57, and 8.30 ± 1.92, respectively. There was no significant difference in the average BMI between the two groups, but a significant difference was observed in the other two parameters.
Additionally, as observed in Table 2, scores for the knowledge, attitude, and practice of participants in the questionnaire were recorded. The average knowledge, attitude, and practice scores in the exposure group were 55.54 ± 13.99, 26.15 ± 14.03, and 41.92 ± 14.69, respectively. These scores in the non-exposure group were 52.56 ± 13.24, 26.01 ± 14.85, and 41.47 ± 15.02, respectively. Although the scores were higher in the exposure group, no statistically significant differences existed in any of the categories.
Discussion
The current study aimed to investigate the effectiveness of nutrition experts' presence on various biochemical parameters, including blood sugar, BMI, awareness, attitude, and practice in patients with type 2 diabetes. The study's results demonstrated that nutrition education provided to the patients led to the control of fasting blood sugar and glycosylated hemoglobin levels. These findings are consistent with previous studies by Sharifi Rad et al. (15) and Kashfi et al. (16), which reported significant reductions in fasting blood sugar levels after nutrition education interventions.
The study did not find a significant difference between the exposure and non-exposure groups regarding BMI as an anthropometric index. This aligns with the findings of Maheri et al. (17), who also observed no significant difference in BMI between the exposure and non-exposure groups in their study. Similarly, there were no significant changes in average weight and waist circumference before and after the educational intervention. However, HbA1c and fasting blood sugar levels significantly decreased in the intervention group, which is consistent with the present study.
Numerous studies have demonstrated the effectiveness of educational interventions in improving the nutritional status of diabetic patients. Studies by Heydari et al. (18) and Gucciardi et al. (19) have shown positive impacts of educational interventions on the nutritional performance of diabetic patients. Thus, educating diabetic patients about proper nutrition and ensuring follow-up can improve their nutritional status.
Considering the importance of a proper diet for type 2 diabetic patients, it is recommended that training courses be organized in healthcare centers and other diabetes-related organizations. Regular training courses conducted by official bodies can yield better results due to the availability of appropriate educational facilities and qualified experts. The significance of continuous education should not be overlooked, as demonstrated by the study conducted at the Yazd Diabetes Center by Baghian Moghadam (20) which showed a significant reduction in HbA1c levels after a five-month educational intervention.
It is important to note that raising awareness about the importance of food and nutrition education alone is not sufficient for diabetes control. Strategies should be implemented to enhance patients' awareness, attitude, and practice. In the present study, there was no significant difference in the knowledge, attitude, and practice scores between the exposure and non-exposure groups. One reason for the decline in scores in the exposure group was the limited utilization of the meal plans provided by the nutritionist. Additionally, the non-exposure group engaged in personal participation in classes, workshops, and media and virtual training, which were not recorded and evaluated. The findings of Mandana Goodarzi et al. (21) on the relationship between knowledge, attitude, practice, and self-efficacy of type 2 diabetic patients somewhat align with the present study's findings.
In summary, the study highlights the effectiveness of nutrition education in controlling blood sugar levels and glycosylated hemoglobin in patients with type 2 diabetes. While no significant changes were observed in BMI, continuous education and comprehensive approaches to improving patients' knowledge, attitude, and practice should be emphasized. Regular training courses by official bodies can play a vital role in enhancing the nutritional status and overall well-being of diabetic patients.
Conclusion
This study's findings demonstrate the effectiveness of educational interventions in reducing fasting blood sugar and HbA1c levels among type 2 diabetic patients in the exposure group compared to the non-exposure group. These results indicate the positive impact of diet and physical activity education on diabetes management. However, further clinical trials are needed to draw more robust conclusions. It is important to note that while other studies have shown improvements in awareness, attitude, and practice, this study did not find significant changes in these scores. Therefore, it is recommended that control, monitoring, and educational follow-up measures be implemented in similar programs.
The outcomes of this research provide a foundation for future studies, including the design and evaluation of educational-supportive interventions.
Acknowledgement
The authors express their gratitude to Golestan University of Medical Sciences for their assistance in recruiting patients for this study.
Funding sources
Golestan University of Medical Sciences approved and funded this research under grant number 113268.
Ethical statement
Approval from the Ethics Committee of Golestan University of Medical Sciences (IR.GOUMS.REC.1401.510) was obtained prior to conducting the study. Consent for participation was obtained from the patients through an opt-out document, ensuring their voluntary involvement.
Conflicts of interest
The authors declare no conflicts of interest associated with this research.
Author contributions
Conceptualization, AGh and MH; methodology, MH; validation, AGh and AM; investigation, AGh and AJ; resources, AGh and JH; data curation, MH and JH; writing-original draft preparation, AGh and AJ; writing-review and editing, MH; visualization, MH; supervision, MH; project administration, MH. All authors have read and agreed to the published version of the manuscript.
References
1. Cole JB, Florez JC. Genetics of diabetes mellitus and diabetes complications. Nat Rev Nephrol. 2020;16(7):377-90. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Lovic D, Piperidou A, Zografou I, Grassos H, Pittaras A, Manolis A. The growing epidemic of diabetes mellitus. Curr Vasc Pharmacol. 2020;18(2):104-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Ojo O. Dietary intake and type 2 diabetes. Nutrients. 2019;11(9):2177. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Cloete L. Diabetes mellitus: an overview of the types, symptoms, complications and management. Nurs Stand. 2022;37(1):61-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Dämon S, Schätzer M, Höfler J, Tomasec G, Hoppichler F. Nutrition and diabetes mellitus: an overview of the current evidence. Wien Med Wochenschr. 2011;161(11-12):282-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Krejčí H, Vyjídák J, Kohutiar M. Low-carbohydrate diet in diabetes mellitus treatment. Vnitr Lek. 2018;64(7-8):742-52. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Isakova DN, Dorodneva EF, Belokrylova LV, Kurmangulov AA, Petrov IM. The role of nutritional factors in the formation of cardiovascular risk in patients with type 2 diabetes mellitus. Vopr Pitan. 2021;90(5):104-14. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Early KB, Stanley K. Position of the Academy of Nutrition and Dietetics: the role of medical nutrition therapy and registered dietitian nutritionists in the prevention and treatment of prediabetes and type 2 diabetes. J Acad Nutr Diet. 2018;118(2):343-53. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Hamdy O, Barakatun-Nisak M-Y. Nutrition in diabetes. Endocrinol Metab Clin North Am. 2016;45(4):799-817. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Custódio JS, Roriz-Filho J, Cavalcanti CAJ, Martins A, Salles JEN. Use of SGLT2 inhibitors in older adults: scientific evidence and practical aspects. Drugs Aging. 2020;37(6):399-409. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Ojo O. Recent advances in nutrition and diabetes. Nutrients. 2021;13(5):1573. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Mitchell LJ, Ball LE, Ross LJ, Barnes KA, Williams LT. Effectiveness of dietetic consultations in primary health care: a systematic review of randomized controlled trials. J Acad Nutr Diet. 2017;117(12):1941-62. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Tahereh Lashkari, Farideh Doostan. The Effect of Clinical Nutrition Education on Blood Glucose and Serum Lipids Control: A Study on Type II Diabetic Patients Referred to Diabetes Center of ShahidBahonar Hospital, Kerman, Iran. Health and Development Journal. 2016;5(1):79-89. [View at Publisher] [Google Scholar]
14. Niroomand M, Ghasemi SN, Karimi-Sari H, Kazempour-Ardebili S, Amiri P, Khosravi MH. Diabetes knowledge, attitude and practice (KAP) study among Iranian in-patients with type-2 diabetes: a cross-sectional study. Diabetes Metab Syndr. 2016;10(1 Suppl 1):S114-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Sharifirad G, Entezari M, Kamran A, Azadbakhat L. Effectiveness of nutrition education to patients with type 2 diabetes: The health belief model. IJDLD. 2008;7(4):379-86. [View at Publisher] [PMID] [Google Scholar]
16. Kashfi SM, Khani jyhouni A, Bahadori khalili R, Hatami M. Evaluation of the effects of educating about nutrition and jogging on the blood sugar of type II diabetic patients of a clinic in Shiraz, Iran. Hakim. 2009;12(3):54-60. [View at Publisher] [Google Scholar]
17. Maheri A, Asnaashari M, Joveini H, Tol A, Firouzian AA, Rohban A. The impact of educational intervention on physical activity, nutrition and laboratory parameters in type II diabetic patients. Electron Physician. 2017;9(4):4207-14. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Heydari G, Moslemi S, Montazerifar F, Heydari M. Efficacy of education on knowledge, attitude & practice of type II diabetic patients in relation to correct nutrition. Zahedan Journal of Research in Medical Sciences. 2002;4(4):207-13. [View at Publisher] [Google Scholar]
19. Gucciardi E, DeMelo M, Lee RN, Grace SL. Assessment of two culturally competent diabetes education methods: individual versus individual plus group education in Canadian Portuguese adults with type 2 diabetes. Ethn Health. 2007;12(2):163-87. [View at Publisher] [DOI] [PMID] [Google Scholar]
20. BaghyaniMoghadam M, Shafiei F, Haydarneia A, Afkhami M. Efficacy of BASNEF model in controlling of diabetic patients in the city of Yazd. Iran. Indian J Community Health. 2005;30(4):144. [View at Publisher] [Google Scholar]
21. Goodarzi M, Ebrahimzadeh I, Rabi A, Saeedipoor B, Asghari Jafarabadi M. Assessment of knowledge, attitude, practice and selfefficacy of diabetic patients in Karaj, Iran. Iranian J Diabetes Lipid Disorders. 2012;11(3):269-81. [View at Publisher] [DOI] [PMID] [Google Scholar]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |