Sun, Nov 30, 2025
[Archive]
Volume 1, Issue 2 (10-2024)
IJHMD 2024, 1(2): 24-28 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ghojoghdordi M, Charkazi A. Barriers to receiving the booster dose of the COVID-19 vaccine among Turkmen people: A Content Analysis Study. IJHMD 2024; 1 (2) :24-28
URL: http://jhd.goums.ac.ir/article-1-33-en.html
URL: http://jhd.goums.ac.ir/article-1-33-en.html
1- East Health Research Center, Gonbad-e-Kavous Health Center, Golestan University of Medical Sciences, Gonbad-e-Kavous, Iran
2- Department of Public Health, School of Health, Golestan University of Medical Sciences, Gorgan, Iran ,rcharkazi@yahoo.com
2- Department of Public Health, School of Health, Golestan University of Medical Sciences, Gorgan, Iran ,
Full-Text [PDF 478 kb]
(458 Downloads)
| Abstract (HTML) (1790 Views)
Full-Text: (1017 Views)
Introduction
Until June 26, 2023, there were 7,612,530 COVID-19 cases in Iran, and the death toll reached 146,295. Also, 65,233,075 first doses of vaccine, 58,629,067 second doses, and 31,727,452 third and higher doses were administered (1). Different studies indicate vaccine effectiveness decreases over time, and boosters are required (1-4).
Several foreign and domestic vaccines were offered to the public as COVID-19 vaccination began. Sinopharm, AstraZeneca, Bharat Biotech, and Sputnik V were the foreign vaccines offered to the public as first and second doses. COVIran Barekat vaccine was the primary domestic vaccine on offer. Later, Sputnik V, AstraZeneca, and Bharat Biotech vaccines were no longer used for different reasons. Still, domestic vaccines such as Soberana (PastoCoVac), Soberana plus (PastoCoVac), SpikoGen ®, and COVIran Barekat replaced them. Currently, these vaccines and the Sinopharm vaccine are offered to the general public.
Vaccine hesitancy is one of the major public health challenges. WHO's strategic advisory group of experts has defined vaccine hesitancy as a delay in acceptance or refusal of vaccination despite the availability of vaccination services, which can differ based on where, when, and how it happens. Studies have discussed this phenomenon, which is different for every vaccine (5-7). Vaccine hesitancy is a great global concern, and in 2019, WHO identified it as one of the 10 most important global health challenges (8,9).
According to the Ministry of Health, public acceptance of third and subsequent COVID-19 doses has significantly decreased compared to the acceptance of the first two doses (10). This disinclination has not been studied in Iran, but studies worldwide suggest different reasons. For example, a study performed in Poland indicated that vaccine side effects and fear are the two primary reasons why COVID-19 booster shots are not complied with (11). A study performed by Yadete et al. in the United States of America indicated that 38 percent of the population was hesitant to use COVID-19 vaccine boosters, primarily due to mistrust of vaccines (12).
A plethora of research has been performed on vaccine hesitancy in Iran, but they mainly focused on the first dose of the vaccine (13,14). There have been no domestic studies on the low acceptance of boosters. Identifying the causes of booster shots' low acceptance rate can help plan necessary interventions and healthcare services. Cultural and tribal factors can be responsible for shaping beliefs about healthcare. Turkmen are a populous minority in north Iran who mainly live in the Golestan province and Gonbad-e-Kavous. Experts report a shallow acceptance of third or subsequent COVID-19 vaccine doses among Turkmen residents of Gonbad-e-Kavous. Therefore, this study aimed to use a qualitative content analysis study to identify the obstacles to booster shot injections among Turkmen residents of Gonbad-e-Kavous and use the study results, technical understandings, and experiences about vaccination to assist healthcare policymakers control the COVID-19 pandemic. This study was designed and performed to illuminate the obstacles to booster injections among Turkmen residents of Gonbad-e-Kavous.
Methods
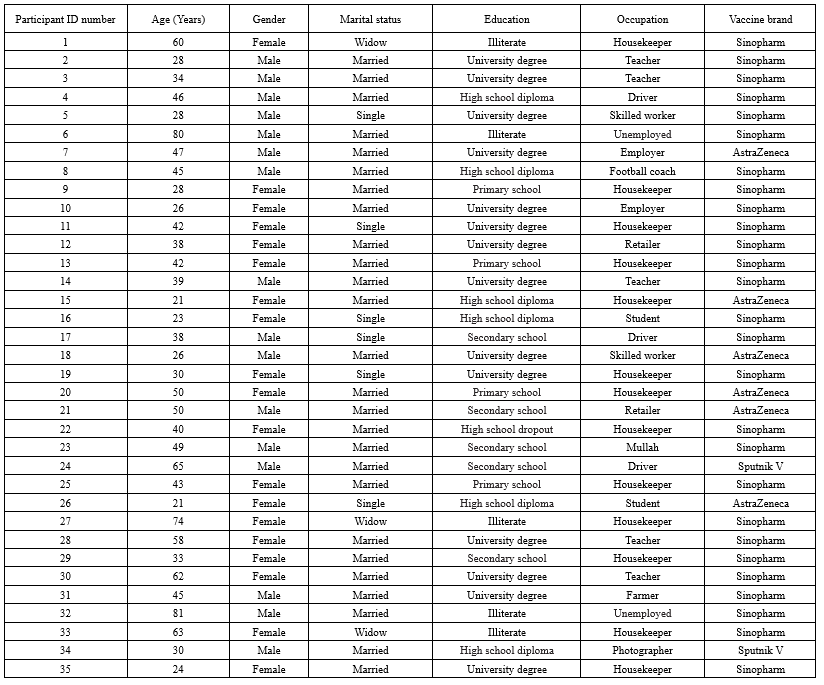
This explorative qualitative study was performed during August and September of 2022 on 35 Turkmen residents of Gonbad-e-Kavous who had not received their third or higher COVID-19 vaccine doses. Sampling was done in a purposive way with utmost diversity. People who had received their first and second doses of vaccine but not the subsequent doses were chosen using the public vaccination system, contacted, and interviewed. After introducing himself and clarifying the study's objectives, the interviewer, a Turkmen resident of Gonbad-e-Kavous who worked at the city's healthcare center, asked the participants why they hadn't received their booster shots. The participants were also asked to discuss their vaccination experiences and explain why they did not complete their vaccination. The next questions were based on the participant's previous answers and the interview guide. The interviews were all recorded, carefully transcribed, prepared, organized, reported, and studied. Our diverse participants included members of both sexes from different ages and educational backgrounds to represent the target population. In the end, the participants' demographic characteristics were recorded in a separate table.
Qualitative analysis methods were used to analyze data. First, the recorded conversations were transcribed and then closely studied to extract their common and general messages. Then, the interviews were organized through open codification. The MAXQDA10 text-organizing software was used to process the extracted codes. Repeated studies on the extracted codes helped organize and spotlight their differences and similarities. Finally, they were analyzed. After each interview, the text was analyzed through content analysis methods. First, units of meaning were identified in the text of each interview (Our study's analysis units). Then, these units of meaning, sentences with the same general meaning, were summarized without losing meaning. The summarized units of meaning were labeled with codes. Different codes were compared based on similarities and differences and then organized into different levels.
Results
The average age of the participants was 43.11 ± 16.51, with an age range of 21-81. Nineteen participants were women (53.4 %), and 26 were married (74.3 %). 14 participants had education beyond diplomas (40 %), 10 participants had no diplomas (28.6 %), 6 participants had diplomas (17.1 %), and 5 participants were uneducated (14.3 %). Most participants had received Sinopharm vaccines (77.1 %) (Table 1).
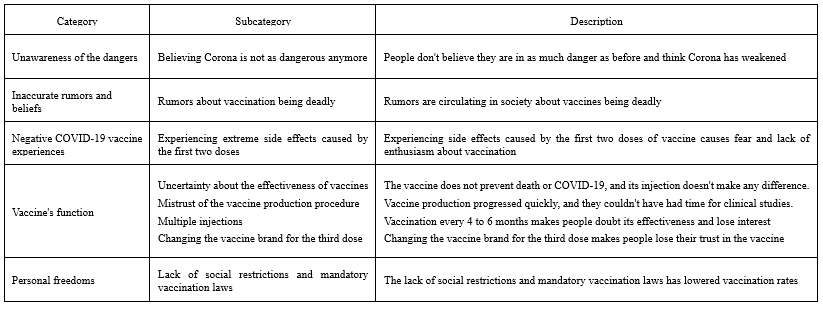
Our findings indicated that there were five main reason categories why our participants had not received their 3rd or subsequent vaccine doses. These levels were (Table 2):
1) Perceived risk
2) Inaccurate information and beliefs
3) Negative COVID-19 vaccine experiences
4) Vaccine effectiveness
5) Personal freedoms
Until June 26, 2023, there were 7,612,530 COVID-19 cases in Iran, and the death toll reached 146,295. Also, 65,233,075 first doses of vaccine, 58,629,067 second doses, and 31,727,452 third and higher doses were administered (1). Different studies indicate vaccine effectiveness decreases over time, and boosters are required (1-4).
Several foreign and domestic vaccines were offered to the public as COVID-19 vaccination began. Sinopharm, AstraZeneca, Bharat Biotech, and Sputnik V were the foreign vaccines offered to the public as first and second doses. COVIran Barekat vaccine was the primary domestic vaccine on offer. Later, Sputnik V, AstraZeneca, and Bharat Biotech vaccines were no longer used for different reasons. Still, domestic vaccines such as Soberana (PastoCoVac), Soberana plus (PastoCoVac), SpikoGen ®, and COVIran Barekat replaced them. Currently, these vaccines and the Sinopharm vaccine are offered to the general public.
Vaccine hesitancy is one of the major public health challenges. WHO's strategic advisory group of experts has defined vaccine hesitancy as a delay in acceptance or refusal of vaccination despite the availability of vaccination services, which can differ based on where, when, and how it happens. Studies have discussed this phenomenon, which is different for every vaccine (5-7). Vaccine hesitancy is a great global concern, and in 2019, WHO identified it as one of the 10 most important global health challenges (8,9).
According to the Ministry of Health, public acceptance of third and subsequent COVID-19 doses has significantly decreased compared to the acceptance of the first two doses (10). This disinclination has not been studied in Iran, but studies worldwide suggest different reasons. For example, a study performed in Poland indicated that vaccine side effects and fear are the two primary reasons why COVID-19 booster shots are not complied with (11). A study performed by Yadete et al. in the United States of America indicated that 38 percent of the population was hesitant to use COVID-19 vaccine boosters, primarily due to mistrust of vaccines (12).
A plethora of research has been performed on vaccine hesitancy in Iran, but they mainly focused on the first dose of the vaccine (13,14). There have been no domestic studies on the low acceptance of boosters. Identifying the causes of booster shots' low acceptance rate can help plan necessary interventions and healthcare services. Cultural and tribal factors can be responsible for shaping beliefs about healthcare. Turkmen are a populous minority in north Iran who mainly live in the Golestan province and Gonbad-e-Kavous. Experts report a shallow acceptance of third or subsequent COVID-19 vaccine doses among Turkmen residents of Gonbad-e-Kavous. Therefore, this study aimed to use a qualitative content analysis study to identify the obstacles to booster shot injections among Turkmen residents of Gonbad-e-Kavous and use the study results, technical understandings, and experiences about vaccination to assist healthcare policymakers control the COVID-19 pandemic. This study was designed and performed to illuminate the obstacles to booster injections among Turkmen residents of Gonbad-e-Kavous.
Methods
This explorative qualitative study was performed during August and September of 2022 on 35 Turkmen residents of Gonbad-e-Kavous who had not received their third or higher COVID-19 vaccine doses. Sampling was done in a purposive way with utmost diversity. People who had received their first and second doses of vaccine but not the subsequent doses were chosen using the public vaccination system, contacted, and interviewed. After introducing himself and clarifying the study's objectives, the interviewer, a Turkmen resident of Gonbad-e-Kavous who worked at the city's healthcare center, asked the participants why they hadn't received their booster shots. The participants were also asked to discuss their vaccination experiences and explain why they did not complete their vaccination. The next questions were based on the participant's previous answers and the interview guide. The interviews were all recorded, carefully transcribed, prepared, organized, reported, and studied. Our diverse participants included members of both sexes from different ages and educational backgrounds to represent the target population. In the end, the participants' demographic characteristics were recorded in a separate table.
Qualitative analysis methods were used to analyze data. First, the recorded conversations were transcribed and then closely studied to extract their common and general messages. Then, the interviews were organized through open codification. The MAXQDA10 text-organizing software was used to process the extracted codes. Repeated studies on the extracted codes helped organize and spotlight their differences and similarities. Finally, they were analyzed. After each interview, the text was analyzed through content analysis methods. First, units of meaning were identified in the text of each interview (Our study's analysis units). Then, these units of meaning, sentences with the same general meaning, were summarized without losing meaning. The summarized units of meaning were labeled with codes. Different codes were compared based on similarities and differences and then organized into different levels.
Results
The average age of the participants was 43.11 ± 16.51, with an age range of 21-81. Nineteen participants were women (53.4 %), and 26 were married (74.3 %). 14 participants had education beyond diplomas (40 %), 10 participants had no diplomas (28.6 %), 6 participants had diplomas (17.1 %), and 5 participants were uneducated (14.3 %). Most participants had received Sinopharm vaccines (77.1 %) (Table 1).
Our findings indicated that there were five main reason categories why our participants had not received their 3rd or subsequent vaccine doses. These levels were (Table 2):
1) Perceived risk
2) Inaccurate information and beliefs
3) Negative COVID-19 vaccine experiences
4) Vaccine effectiveness
5) Personal freedoms
Perceived risk
One of the extracted levels is ignorance of the dangers of COVID-19. Some participants believed that the COVID-19 virus had weakened and was not as dangerous as it used to be. Consequently, they had no reason to receive their boosters. The opinion of one of the participants regarding this issue was:
"We have no intention to get our third and fourth vaccine doses. It has been so long since our second dose. We were among the first people to get the second dose last summer. We are not going to get the other doses. There is no Corona anymore. Our lives are not in danger. We are very healthy."
Why haven't you received the third and fourth vaccine doses?
" As I said, there's no problem anymore. Our lives are back to normal; we have no more problems. We don't see a need for it anymore. Right now, it seems like the storm has passed us. Things are back to normal." (Participant #2).
Another participant said:
"We were very enthusiastic about the first and second doses. Back then, the disease was very dangerous. Right now, the situation has improved, thank goodness. Things are safe and sound. The new variance was not very intense either; it was a simple cold and runny nose…. The situation in our village is okay right now, thank goodness. I don't know about the city. It's not like it used to be. Back then, one side of the cemetery was filled in a short time. It's not like that anymore, Thank goodness." (Participant#14).
Inaccurate rumors and beliefs
Inaccurate rumors and beliefs formed another one of the extracted levels. Many participants believed vaccination caused death. For example:
" A young boy lost his life when he got vaccinated. He died two days after vaccination. He was my son's friend. He didn't continue his vaccination because of that. Neither did I." (Participant #1)
Another one of the participants said:
"To be honest, I'm scared to have the third dose. My cousin died because of this last week."
After he had his vaccine injected?
"Yes. The poor soul had it injected. He died last week. Because of that, I'm scared to go near vaccines. Our entire neighborhood is talking about how he died because of the Corona vaccine. His wife is crying out loud, begging people not to get vaccinated. It's so unfortunate. His time was up, right? He didn't even have any other diseases. He was a healthy boy. Very healthy. He was an employee. A rental driver. He would leave for work early in the morning and return late at night. He left three kids behind." (Participant #14)
Participant #18 said:
"We're not getting it for now. Three of my neighbors got the vaccine and died. I'm not doing it yet."
Participant #21 believed:
"As you know, people say vaccines kill people. So, I thought I shouldn't dig my own grave with my own hands and didn't continue with the vaccination. I told myself we won't get Corona, and fortunately, we're still healthy. But when we got vaccinated, we got sick. Even though we were completely healthy before the vaccine, we got sick after it."
Another rumor says that vaccination exacerbates other diseases and physical issues and intensifies them. One of the participants said:
"They say vaccines reveal any diseases you might have in your body. And I got scared. I had already had two doses." (Participant #13).
Negative COVID-19 vaccine experiences
Negative COVID-19 vaccine experiences, especially negative experiences from the second dose, were the major obstacles to complete vaccination and were repeated by the participants numerous times. Negative severe side effects caused by previous doses created mistrust and fear of vaccination among our participants and prevented their complete vaccination. One participant said:
"I have migraines, which get bad sometimes. Before vaccination, it used to get bad once every two or three weeks, but after I got vaccinated, it got bad every day or every other day. I don't have other specific reasons." (Participant #3)
Another participant said:
"My family and I are always in pain and fatigued. Four family members were ready for vaccination, and we had two doses. My family is fatigued like me, too. I personally always have a fatigued and hurting body. My wife also has pains which won't go away."
Did all this start after you get vaccinated?
"Yes, it started after the second dose. The first dose didn't have any side effects. But the second dose caused fatigue, muscular pains, and overall pains. We took multivitamins effervescent tablets. The symptoms would go away periodically, but they would always come back. That's why we didn't continue with the rest of the doses. We didn't want any more problems." (Participant #22)
Observing intense side effects on acquaintances was a sublevel of this level, which many participants mentioned. One participant said:
"Well, I had the first and second doses. I was waiting to get the third dose when my neighbor took their third dose. There was another disease going around back then, too, the Omicron. After getting the third dose, they started experiencing shortness of breath. I was afraid it would happen to me, too, so I didn't continue with the vaccination. We were cleared for our third dose almost at the same time. My neighbor took it first, and all of that happened, which scared me. I had already had the first and second doses but didn't go for the third and fourth. I was scared. That's why I didn't continue." (Participant #9)
Vaccine effectiveness
Another level extracted in this study was vaccine effectiveness. Four of this level's sublevels were uncertainties about vaccine effectiveness, mistrust of the vaccine production procedure, numerous injections, and changing the vaccine brand for the third dose.
Some of our participants believed that vaccine injection did nothing to prevent death or Corona. One participant said:
"Injecting it or not doesn't matter. Vaccinated people die, too. The ones who didn't get vaccinated are living normal lives. Some people didn't even have the first and second doses. I believe people can't say they're completely safe since they've gotten vaccinated. Even vaccinated people die. You're not safe after getting vaccinated.” (Participant #5)
Another participant said:
"I got Corona after having the first and second doses. They didn't have any effects. I got the virus again after getting two shots of the vaccine. That was the second time. First, I got it after the first dose, and then again, I got it after the second dose." (Participant #7)
People mistrusted the high speed of vaccine production. People had negative opinions about how fast vaccines are being produced. One of the participants said:
"In my opinion, vaccines should be thoroughly tested first. Then, they should inject it into people. They haven't tested these vaccines, have they? They made a vaccine in a short time and are forcing people to have it injected. But it's not a vaccine that has been tested and experienced for a long time. I think the Corona vaccine isn't like that. That's my opinion, though. Am I right? They haven't tested it." (Participant #30)
Multiple injections every few months were another reason people didn't want the third and fourth doses. One of the participants said:
"They say you have to keep getting more and more doses every time. Like after a few months you'll have to take the third, fourth, fifth, and even sixth dose. They say that's what it's going to be like. And they say it's harmful." (Participant #4)
Another participant said:
"They say it loses its effectiveness over time, and you have to keep taking it. For example, we would have to get vaccinated every month. They say that has side effects. That's why I'm not continuing with it." (Participant #16)
Changing the vaccine brand for the third dose was another sublevel mentioned by a few participants. Participant #24 said:
"When we went to have our third dose, they didn't have our vaccine anymore. They said we should take another brand. But we didn't. I said if they have Sputnik V we'll have it, we don't want the other brands. And we didn't continue with our vaccination after that."
Personal freedoms
Personal freedom was another level extracted in this study. Since vaccination was not mandatory and social restrictions on unvaccinated people had been lifted, people had been less enthusiastic about their remaining vaccine doses. One participant said:
"As long as it is not mandatory, I won't have it. I believe they should make people have their vaccination cards when going around. If vaccination cards are necessary, people will get vaccinated." (Participant #16)
Discussion
Vaccine hesitancy presents a significant health challenge. This challenge has recently grown due to the COVID-19 pandemic, its vaccination, and multiple vaccine doses. This study aimed to identify obstacles that prevented receiving third and fourth COVID-19 vaccine doses among Turkmen residents of Gonbad-e-Kavous City. Ultimately, five primary levels were identified, which will be discussed below.
Perceived risk
One of the main reasons the public did not accept booster COVID-19 vaccine shots was underestimating the dangers of COVID-19. Most participants believed the disease had lessened, and the danger of a severe and deadly virus was behind them. This was true to some extent, and the mortality rates of the previous months indicated that the disease had gotten weaker. This can be attributed to widespread public vaccination. In the summer of 2021, people were enthusiastic about receiving the first and second vaccine doses due to the Delta variant claiming many lives. That enthusiasm led to widespread vaccination, which strengthened the public's immunity levels against the disease. According to healthcare guidelines about understood threats, when people consider themselves vulnerable to a very severe and deadly disease, they will take preventative measures against it (15). In the case of COVID-19, which had a high spreading rate and was severe and deadly, the death of acquaintances forced people to seek vaccination and preventative measures personally. The results of Denis et al.'s study indicated that unawareness of the dangers of the disease resulted in low vaccination rates among British healthcare workers (16). Therefore, people believed the disease weakened, and they saw no reason to get vaccinated. The results of Rzymski et al.'s study in Poland indicated that people who were hesitant about getting their booster shots did not believe it was necessary (11). The results of the study performed by Wang et al. and Harapan et al. indicated that vaccination rates among people who were aware of possible dangers were twice the vaccination rates of the unaware (17,18).
Inaccurate rumors and beliefs
Many participants mentioned negative rumors and stories as the primary obstacles against vaccination. The most common rumor was death after the third dose. This myth was circulated among Turkmen city residents, became a solid belief, and prevented vaccination. Healthcare policymakers must engage through various channels to rebuild public trust against this myth. Inaccurate information about health threats is a significant threat to the public health (19). This pandemic brought with it a vast amount of misinformation about the characteristics of the disease, its nature, its spreading, preventative measures, and remedies, which damaged the public's trust in healthcare authorities (20,21). Fake news comprises a wide variety of misleading, purposefully included or excluded, accidental or false, and altered information. Fake news combines false information and intentional lies (22). WHO announced that healthcare systems were not facing a pandemic but an infodemic (23).
Studies indicate that fake news and rumors negatively affect public vaccination acceptance; those who recognize inaccurate information are more likely to accept vaccination (24-26). Therefore, the public must be educated about the COVID-19 vaccine to recognize erroneous information about it. Healthcare media should provide scientific and persuasive responses to inaccurate information to raise public awareness.
Negative COVID-19 vaccine experiences
Another important factor identified in our study was negative experiences caused by first and second vaccine doses. Severe side effects caused by the previous two doses caused vaccine hesitancy. Many studies have confirmed the fear of short-term side effects caused by COVID-19 vaccines (13,24,25). In the study by Rzymski et al., adverse side effects of the previous dose were the most significant reason people didn't want the booster shot (11). It must always be remembered that all vaccines may have side effects. Healthcare authorities should educate the public about these side effects and how to manage them. This will help people understand vaccination and its side effects and alleviate their fears.
Vaccine effectiveness
Vaccine effectiveness was another extracted level. Some participants believed vaccines were ineffective and that they did not prevent COVID-19 infection. Some people reported being reinfected with the virus despite vaccination, which they viewed as ineffective. Some believed that the fact that multiple vaccine doses were required showed ineffectiveness and meant vaccination was pointless. Other studies have indicated that people did not trust the coronavirus vaccines (26-29). The study's results by Khankeh et al. indicated that people did not trust the effectiveness of vaccines, which decreased public compliance with vaccination (13).
People also believed that the fast production rates of COVID-19 vaccines indicated their ineffectiveness. Some participants highlighted the fast production rates of COVID-19 vaccines and believed that the researchers had no time to perform clinical tests and experiments on them. Other studies also emphasized this problem (14,28-32).
Some participants mentioned not continuing vaccination because they had to change the vaccine brand they had taken for the first two doses. For example, some participants had AstraZeneca or Sputnik V vaccines for their first two doses but were recommended a different brand for their third dose. This problem was caused by removing those vaccine brands from the public vaccination system and replacing them with different brands. This change might have decreased public enthusiasm toward vaccination. To restore public trust, healthcare authorities must provide scientific and convincing evidence of the new brands' effectiveness and clarify why the old ones were replaced.
Personal freedoms
Another extracted level was personal freedom. The lack of social restrictions on unvaccinated people and mandatory vaccination laws reduced the public enthusiasm toward booster doses compared to the first two doses. In 2021, many Iranian governmental organizations did not provide services to unvaccinated people, which forced people to get vaccinated. But lately, these restrictions have been lifted, and mandatory vaccination laws are no longer in place, which caused some people not to continue vaccinating. The results of the study performed by Torabi and Sotodeh on students at Shiraz University in Iran indicated that many students received the vaccine due to public pressure rather than their personal desire for it (33).
Study strengths
This study has several advantages that should be noted. First, it is a qualitative study that reveals the participants' deepest concerns and beliefs. Second, the interviews were performed through phone calls, resulting in better, more honest answers than face-to-face interviews. Third, our participants had already received two doses of vaccines but had not continued with their vaccination, which helped us find out why public enthusiasm toward vaccination decreased after the second dose. All this helped us provide healthcare policymakers with clear insights.
Study limitations
The qualitative nature of the study limited the potential of generalizing the results. Social pressures and orientations might have affected the data collected by our team. To minimize this effect, our interviewer explained the goals of our study before beginning the interview and assured the participants of their anonymity. The third limitation was that this study was performed on Turkmen citizens. Other groups of people might have had different opinions and beliefs.
Conclusion
This study identified five barriers in different categories that prevented third and subsequent COVID-19 vaccine injections among Turkmen citizens: perceived risk, inaccurate rumors and beliefs, negative COVID-19 vaccine experiences, vaccine effectiveness, and personal freedoms.
Educational interventions are essential to enhance public awareness about the dangers of COVID-19, combat misinformation regarding vaccinations, inform citizens about vaccine side effects, restore Turkmen citizens' trust, and boost their motivation for COVID-19 booster shots. Similar studies on other groups in other regions of our country can better help identify the obstacles against COVID-19 vaccination and provide healthcare authorities with proper guidelines to design interventions and increase acceptance of COVID-19 vaccine boosters.
Acknowledgement
The authors would like to express their gratitude to all the participants who participated in the study.
Funding sources
The funding for this study was provided by Golestan University of Medical Sciences.
Ethical statement
This study was approved by the Golestan Medical University's technology and research group's moral committee and given the following identifying code: IR.GOLESTAN.REC.1401.272.
Conflicts of interest
The authors declare that there is no conflict of interest.
Author contributions
MG: data gathering, conceptualization, analysis, and draft preparation. AC: study design, analysis, data interpretation, and writing. All authors read and approved the final manuscript.
One of the extracted levels is ignorance of the dangers of COVID-19. Some participants believed that the COVID-19 virus had weakened and was not as dangerous as it used to be. Consequently, they had no reason to receive their boosters. The opinion of one of the participants regarding this issue was:
"We have no intention to get our third and fourth vaccine doses. It has been so long since our second dose. We were among the first people to get the second dose last summer. We are not going to get the other doses. There is no Corona anymore. Our lives are not in danger. We are very healthy."
Why haven't you received the third and fourth vaccine doses?
" As I said, there's no problem anymore. Our lives are back to normal; we have no more problems. We don't see a need for it anymore. Right now, it seems like the storm has passed us. Things are back to normal." (Participant #2).
Another participant said:
"We were very enthusiastic about the first and second doses. Back then, the disease was very dangerous. Right now, the situation has improved, thank goodness. Things are safe and sound. The new variance was not very intense either; it was a simple cold and runny nose…. The situation in our village is okay right now, thank goodness. I don't know about the city. It's not like it used to be. Back then, one side of the cemetery was filled in a short time. It's not like that anymore, Thank goodness." (Participant#14).
Inaccurate rumors and beliefs
Inaccurate rumors and beliefs formed another one of the extracted levels. Many participants believed vaccination caused death. For example:
" A young boy lost his life when he got vaccinated. He died two days after vaccination. He was my son's friend. He didn't continue his vaccination because of that. Neither did I." (Participant #1)
Another one of the participants said:
"To be honest, I'm scared to have the third dose. My cousin died because of this last week."
After he had his vaccine injected?
"Yes. The poor soul had it injected. He died last week. Because of that, I'm scared to go near vaccines. Our entire neighborhood is talking about how he died because of the Corona vaccine. His wife is crying out loud, begging people not to get vaccinated. It's so unfortunate. His time was up, right? He didn't even have any other diseases. He was a healthy boy. Very healthy. He was an employee. A rental driver. He would leave for work early in the morning and return late at night. He left three kids behind." (Participant #14)
Participant #18 said:
"We're not getting it for now. Three of my neighbors got the vaccine and died. I'm not doing it yet."
Participant #21 believed:
"As you know, people say vaccines kill people. So, I thought I shouldn't dig my own grave with my own hands and didn't continue with the vaccination. I told myself we won't get Corona, and fortunately, we're still healthy. But when we got vaccinated, we got sick. Even though we were completely healthy before the vaccine, we got sick after it."
Another rumor says that vaccination exacerbates other diseases and physical issues and intensifies them. One of the participants said:
"They say vaccines reveal any diseases you might have in your body. And I got scared. I had already had two doses." (Participant #13).
Negative COVID-19 vaccine experiences
Negative COVID-19 vaccine experiences, especially negative experiences from the second dose, were the major obstacles to complete vaccination and were repeated by the participants numerous times. Negative severe side effects caused by previous doses created mistrust and fear of vaccination among our participants and prevented their complete vaccination. One participant said:
"I have migraines, which get bad sometimes. Before vaccination, it used to get bad once every two or three weeks, but after I got vaccinated, it got bad every day or every other day. I don't have other specific reasons." (Participant #3)
Another participant said:
"My family and I are always in pain and fatigued. Four family members were ready for vaccination, and we had two doses. My family is fatigued like me, too. I personally always have a fatigued and hurting body. My wife also has pains which won't go away."
Did all this start after you get vaccinated?
"Yes, it started after the second dose. The first dose didn't have any side effects. But the second dose caused fatigue, muscular pains, and overall pains. We took multivitamins effervescent tablets. The symptoms would go away periodically, but they would always come back. That's why we didn't continue with the rest of the doses. We didn't want any more problems." (Participant #22)
Observing intense side effects on acquaintances was a sublevel of this level, which many participants mentioned. One participant said:
"Well, I had the first and second doses. I was waiting to get the third dose when my neighbor took their third dose. There was another disease going around back then, too, the Omicron. After getting the third dose, they started experiencing shortness of breath. I was afraid it would happen to me, too, so I didn't continue with the vaccination. We were cleared for our third dose almost at the same time. My neighbor took it first, and all of that happened, which scared me. I had already had the first and second doses but didn't go for the third and fourth. I was scared. That's why I didn't continue." (Participant #9)
Vaccine effectiveness
Another level extracted in this study was vaccine effectiveness. Four of this level's sublevels were uncertainties about vaccine effectiveness, mistrust of the vaccine production procedure, numerous injections, and changing the vaccine brand for the third dose.
Some of our participants believed that vaccine injection did nothing to prevent death or Corona. One participant said:
"Injecting it or not doesn't matter. Vaccinated people die, too. The ones who didn't get vaccinated are living normal lives. Some people didn't even have the first and second doses. I believe people can't say they're completely safe since they've gotten vaccinated. Even vaccinated people die. You're not safe after getting vaccinated.” (Participant #5)
Another participant said:
"I got Corona after having the first and second doses. They didn't have any effects. I got the virus again after getting two shots of the vaccine. That was the second time. First, I got it after the first dose, and then again, I got it after the second dose." (Participant #7)
People mistrusted the high speed of vaccine production. People had negative opinions about how fast vaccines are being produced. One of the participants said:
"In my opinion, vaccines should be thoroughly tested first. Then, they should inject it into people. They haven't tested these vaccines, have they? They made a vaccine in a short time and are forcing people to have it injected. But it's not a vaccine that has been tested and experienced for a long time. I think the Corona vaccine isn't like that. That's my opinion, though. Am I right? They haven't tested it." (Participant #30)
Multiple injections every few months were another reason people didn't want the third and fourth doses. One of the participants said:
"They say you have to keep getting more and more doses every time. Like after a few months you'll have to take the third, fourth, fifth, and even sixth dose. They say that's what it's going to be like. And they say it's harmful." (Participant #4)
Another participant said:
"They say it loses its effectiveness over time, and you have to keep taking it. For example, we would have to get vaccinated every month. They say that has side effects. That's why I'm not continuing with it." (Participant #16)
Changing the vaccine brand for the third dose was another sublevel mentioned by a few participants. Participant #24 said:
"When we went to have our third dose, they didn't have our vaccine anymore. They said we should take another brand. But we didn't. I said if they have Sputnik V we'll have it, we don't want the other brands. And we didn't continue with our vaccination after that."
Personal freedoms
Personal freedom was another level extracted in this study. Since vaccination was not mandatory and social restrictions on unvaccinated people had been lifted, people had been less enthusiastic about their remaining vaccine doses. One participant said:
"As long as it is not mandatory, I won't have it. I believe they should make people have their vaccination cards when going around. If vaccination cards are necessary, people will get vaccinated." (Participant #16)
Discussion
Vaccine hesitancy presents a significant health challenge. This challenge has recently grown due to the COVID-19 pandemic, its vaccination, and multiple vaccine doses. This study aimed to identify obstacles that prevented receiving third and fourth COVID-19 vaccine doses among Turkmen residents of Gonbad-e-Kavous City. Ultimately, five primary levels were identified, which will be discussed below.
Perceived risk
One of the main reasons the public did not accept booster COVID-19 vaccine shots was underestimating the dangers of COVID-19. Most participants believed the disease had lessened, and the danger of a severe and deadly virus was behind them. This was true to some extent, and the mortality rates of the previous months indicated that the disease had gotten weaker. This can be attributed to widespread public vaccination. In the summer of 2021, people were enthusiastic about receiving the first and second vaccine doses due to the Delta variant claiming many lives. That enthusiasm led to widespread vaccination, which strengthened the public's immunity levels against the disease. According to healthcare guidelines about understood threats, when people consider themselves vulnerable to a very severe and deadly disease, they will take preventative measures against it (15). In the case of COVID-19, which had a high spreading rate and was severe and deadly, the death of acquaintances forced people to seek vaccination and preventative measures personally. The results of Denis et al.'s study indicated that unawareness of the dangers of the disease resulted in low vaccination rates among British healthcare workers (16). Therefore, people believed the disease weakened, and they saw no reason to get vaccinated. The results of Rzymski et al.'s study in Poland indicated that people who were hesitant about getting their booster shots did not believe it was necessary (11). The results of the study performed by Wang et al. and Harapan et al. indicated that vaccination rates among people who were aware of possible dangers were twice the vaccination rates of the unaware (17,18).
Inaccurate rumors and beliefs
Many participants mentioned negative rumors and stories as the primary obstacles against vaccination. The most common rumor was death after the third dose. This myth was circulated among Turkmen city residents, became a solid belief, and prevented vaccination. Healthcare policymakers must engage through various channels to rebuild public trust against this myth. Inaccurate information about health threats is a significant threat to the public health (19). This pandemic brought with it a vast amount of misinformation about the characteristics of the disease, its nature, its spreading, preventative measures, and remedies, which damaged the public's trust in healthcare authorities (20,21). Fake news comprises a wide variety of misleading, purposefully included or excluded, accidental or false, and altered information. Fake news combines false information and intentional lies (22). WHO announced that healthcare systems were not facing a pandemic but an infodemic (23).
Studies indicate that fake news and rumors negatively affect public vaccination acceptance; those who recognize inaccurate information are more likely to accept vaccination (24-26). Therefore, the public must be educated about the COVID-19 vaccine to recognize erroneous information about it. Healthcare media should provide scientific and persuasive responses to inaccurate information to raise public awareness.
Negative COVID-19 vaccine experiences
Another important factor identified in our study was negative experiences caused by first and second vaccine doses. Severe side effects caused by the previous two doses caused vaccine hesitancy. Many studies have confirmed the fear of short-term side effects caused by COVID-19 vaccines (13,24,25). In the study by Rzymski et al., adverse side effects of the previous dose were the most significant reason people didn't want the booster shot (11). It must always be remembered that all vaccines may have side effects. Healthcare authorities should educate the public about these side effects and how to manage them. This will help people understand vaccination and its side effects and alleviate their fears.
Vaccine effectiveness
Vaccine effectiveness was another extracted level. Some participants believed vaccines were ineffective and that they did not prevent COVID-19 infection. Some people reported being reinfected with the virus despite vaccination, which they viewed as ineffective. Some believed that the fact that multiple vaccine doses were required showed ineffectiveness and meant vaccination was pointless. Other studies have indicated that people did not trust the coronavirus vaccines (26-29). The study's results by Khankeh et al. indicated that people did not trust the effectiveness of vaccines, which decreased public compliance with vaccination (13).
People also believed that the fast production rates of COVID-19 vaccines indicated their ineffectiveness. Some participants highlighted the fast production rates of COVID-19 vaccines and believed that the researchers had no time to perform clinical tests and experiments on them. Other studies also emphasized this problem (14,28-32).
Some participants mentioned not continuing vaccination because they had to change the vaccine brand they had taken for the first two doses. For example, some participants had AstraZeneca or Sputnik V vaccines for their first two doses but were recommended a different brand for their third dose. This problem was caused by removing those vaccine brands from the public vaccination system and replacing them with different brands. This change might have decreased public enthusiasm toward vaccination. To restore public trust, healthcare authorities must provide scientific and convincing evidence of the new brands' effectiveness and clarify why the old ones were replaced.
Personal freedoms
Another extracted level was personal freedom. The lack of social restrictions on unvaccinated people and mandatory vaccination laws reduced the public enthusiasm toward booster doses compared to the first two doses. In 2021, many Iranian governmental organizations did not provide services to unvaccinated people, which forced people to get vaccinated. But lately, these restrictions have been lifted, and mandatory vaccination laws are no longer in place, which caused some people not to continue vaccinating. The results of the study performed by Torabi and Sotodeh on students at Shiraz University in Iran indicated that many students received the vaccine due to public pressure rather than their personal desire for it (33).
Study strengths
This study has several advantages that should be noted. First, it is a qualitative study that reveals the participants' deepest concerns and beliefs. Second, the interviews were performed through phone calls, resulting in better, more honest answers than face-to-face interviews. Third, our participants had already received two doses of vaccines but had not continued with their vaccination, which helped us find out why public enthusiasm toward vaccination decreased after the second dose. All this helped us provide healthcare policymakers with clear insights.
Study limitations
The qualitative nature of the study limited the potential of generalizing the results. Social pressures and orientations might have affected the data collected by our team. To minimize this effect, our interviewer explained the goals of our study before beginning the interview and assured the participants of their anonymity. The third limitation was that this study was performed on Turkmen citizens. Other groups of people might have had different opinions and beliefs.
Conclusion
This study identified five barriers in different categories that prevented third and subsequent COVID-19 vaccine injections among Turkmen citizens: perceived risk, inaccurate rumors and beliefs, negative COVID-19 vaccine experiences, vaccine effectiveness, and personal freedoms.
Educational interventions are essential to enhance public awareness about the dangers of COVID-19, combat misinformation regarding vaccinations, inform citizens about vaccine side effects, restore Turkmen citizens' trust, and boost their motivation for COVID-19 booster shots. Similar studies on other groups in other regions of our country can better help identify the obstacles against COVID-19 vaccination and provide healthcare authorities with proper guidelines to design interventions and increase acceptance of COVID-19 vaccine boosters.
Acknowledgement
The authors would like to express their gratitude to all the participants who participated in the study.
Funding sources
The funding for this study was provided by Golestan University of Medical Sciences.
Ethical statement
This study was approved by the Golestan Medical University's technology and research group's moral committee and given the following identifying code: IR.GOLESTAN.REC.1401.272.
Conflicts of interest
The authors declare that there is no conflict of interest.
Author contributions
MG: data gathering, conceptualization, analysis, and draft preparation. AC: study design, analysis, data interpretation, and writing. All authors read and approved the final manuscript.
Type of Study: Original Article |
Subject:
Clinical
Received: 2024/02/7 | Accepted: 2024/10/22 | Published: 2024/12/25
Received: 2024/02/7 | Accepted: 2024/10/22 | Published: 2024/12/25
References
1. COVID-19 and Vaccination Against It in Iran. Ministry of Health and Medical Education. 2022. [View at Publisher]
2. Loubet P, Laureillard D, Martin A, Larcher R, Sotto A. Why promoting a COVID-19 vaccine booster dose? Anaesth Crit Care Pain Med. 2021;40(6):100967. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Andrews N, Stowe J, Kirsebom F, Toffa S, Rickeard T, Gallagher E, et al. Covid-19 vaccine effectiveness against the Omicron (B. 1.1. 529) variant. N Engl J Med. 2022;386(16):1532-46. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Moreira Jr ED, Kitchin N, Xu X, Dychter SS, Lockhart S, Gurtman A, et al. Safety and efficacy of a third dose of BNT162b2 COVID-19 vaccine. N Engl J Med. 2022;386(20):1910-21. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Burki T. Booster shots for COVID-19-the debate continues. Lancet Infect Dis. 2021;21(10):1359-60. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. MacDonald NE. SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161-4. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Karafillakis E, Larson HJ, ADVANCE consortium. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine. 2017;35(37):4840-50. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Cobos Muñoz D, Monzón Llamas L, Bosch-Capblanch X. Exposing concerns about vaccination in low-and middle-income countries: a systematic review. Int J Public Health. 2015;60(7):767-80. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. European Parliament. European Parliament Resolution of 19 April 2018 on Vaccine Hesitancy and Drop in Vaccination Rates in Europe (2017/2951 RSP). 2018. [View at Publisher]
10. WHO. World Health Organization Ten threats to global health in 2019. [View at Publisher]
11. Rzymski P, Poniedziałek B, Fal A. Willingness to receive the booster COVID-19 vaccine dose in Poland. Vaccines. 2021;9(11):1286. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Yadete T, Batra K, Netski DM, Antonio S, Patros MJ, Bester JC. Assessing acceptability of COVID-19 vaccine booster dose among adult Americans: A cross-sectional study. Vaccines. 2021;9(12):1424. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Khankeh HR, Farrokhi M, Khanjani MS, Momtaz YA, Forouzan AS, Norouzi M, et al. The Barriers, Challenges, and Strategies of COVID-19 (SARS-CoV-2) Vaccine Acceptance: A Concurrent Mixed-Method Study in Tehran City, Iran. Vaccines. 2021;9(11):1248. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Lebni JY, Irandoost SF, Sedighi S, Ahmadi S, Hosseini R. Identifying the determinants of non-injection of covid-19 vaccine: A qualitative study in Urmia, Iran. Front Public Health. 2022;10:927400. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Glanz K, Rimer BK, Viswanath K. Health behavior and health education: theory, research, and practice. USA:John Wiley & Sons;2008. [View at Publisher] [Google Scholar]
16. Dennis A, Robin C, Jones LF, Carter H. Exploring vaccine hesitancy in care home employees in North West England: a qualitative study. BMJ Open. 2022;12(5):e055239. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Wang J, Lu X, Lai X, Lyu Y, Zhang H, Fenghuang Y, et al. The changing acceptance of COVID-19 vaccination in different epidemic phases in China: a longitudinal study. Vaccines. 2021;9(3):191. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, et al. Acceptance of a COVID-19 vaccine in Southeast Asia: a cross-sectional study in Indonesia. Front Public Health. 2020;8:381. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Montagni I, Ouazzani-Touhami K, Mebarki A, Texier N, Schück S, Tzourio C, et al. Acceptance of a Covid-19 vaccine is associated with ability to detect fake news and health literacy. J Public Health. 2021;43(4):695-702. [View at Publisher] [DOI] [PMID] [Google Scholar]
20. Ahmed W, Vidal-Alaball J, Downing J, Seguí FL. COVID-19 and the 5G conspiracy theory: social network analysis of Twitter data. J Med Internet Res. 2020;22(5):e19458. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Walter N, Brooks JJ, Saucier CJ, Suresh S. Evaluating the impact of attempts to correct health misinformation on social media: A meta-analysis. Health Commun. 2021;36(13):1776-84. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Siebenhaar KU, Köther AK, Alpers GW. Dealing with the COVID-19 infodemic: Distress by information, information avoidance, and compliance with preventive measures. Front Psychol. 2020;11:567905. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. WHO. Infodemic management: an overview of infodemic management during COVID-19, January 2020-May 2021. 2021. [View at Publisher] [Google Scholar]
24. Lyu H, Zheng Z, Luo J. Both rates of fake news and fact-based news on twitter negatively Correlate with the state-level COVID-19 vaccine uptake. arXiv preprint [PPR: PPR362191]:2021. [View at Publisher] [Google Scholar]
25. Islam MS, Kamal A-HM, Kabir A, Southern DL, Khan SH, Hasan SM, et al. COVID-19 vaccine rumors and conspiracy theories: The need for cognitive inoculation against misinformation to improve vaccine adherence. PLoS One. 2021;16(5):e0251605. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Jemielniak D, Krempovych Y. An analysis of AstraZeneca COVID-19 vaccine misinformation and fear mongering on Twitter. Public Health. 2021;200:4-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
27. Cahapay MB. To get or not to get: Examining the intentions of Philippine teachers to vaccinate against COVID-19. J Hum Behav Soc. 2022;32(3):325-35. [View at Publisher] [DOI] [Google Scholar]
28. van Summeren J, Meijer A, Aspelund G, Casalegno JS, Erna G, Hoang U, et al. Low levels of respiratory syncytial virus activity in Europe during the 2020/21 season: what can we expect in the coming summer and autumn/winter? Euro Surveill. 2021;26(29):2100639. [View at Publisher] [DOI] [PMID] [Google Scholar]
29. Lockyer B, Islam S, Rahman A, Dickerson J, Pickett K, Sheldon T, et al. Understanding COVID-19 misinformation and vaccine hesitancy in context: Findings from a qualitative study involving citizens in Bradford, UK. Health Expect. 2021;24(4):1158-67. [View at Publisher] [DOI] [PMID] [Google Scholar]
30. Woodhead C, Onwumere J, Rhead R, Bora-White M, Chui Z, Clifford N, et al. Race, ethnicity and COVID-19 vaccination: a qualitative study of UK healthcare staff. Ethn Health. 2022;27(7):1555-74. [View at Publisher] [DOI] [PMID] [Google Scholar]
31. Kumari A, Ranjan P, Chopra S, Kaur D, Kaur T, Kalanidhi KB, et al. What Indians Think of the COVID-19 vaccine: A qualitative study comprising focus group discussions and thematic analysis. Diabetes Metab Syndr. 2021;15(3):679-82. [View at Publisher] [DOI] [PMID] [Google Scholar]
32. Duong MC, Nguyen HT, Duong M. Evaluating COVID-19 vaccine hesitancy: A qualitative study from Vietnam. Diabetes Metab Syndr. 2022;16(1):102363. [View at Publisher] [DOI] [PMID] [Google Scholar]
33. Wang J, Ji Q, Dong S, Zhao S, Li X, Zhu Q, et al. Factors Influencing Vaccine Hesitancy in China: A Qualitative Study. Vaccines. 2021;9(11):1291. [View at Publisher] [DOI] [PMID] [Google Scholar]
34. Küçükali H, Ataç Ö, Palteki AS, Tokaç AZ, Hayran O. Vaccine hesitancy and anti-vaccination attitudes during the start of COVID-19 vaccination program: a content analysis on twitter data. Vaccines. 2022;10(2):161. [View at Publisher] [DOI] [PMID] [Google Scholar]
35. Siu JY-m, Cao Y, Shum DH. Perceptions of and hesitancy toward COVID-19 vaccination in older Chinese adults in Hong Kong: A qualitative study. BMC Geriatr. 2022;22(1):288. [View at Publisher] [DOI] [PMID] [Google Scholar]
36. Torabi M, Sotudeh H. The Role of Risk Perception and Ability to Detect Fake News in Acceptance of COVID-19 Vaccine among Students of Shiraz University, Iran. Health Inf Manag. 2022;18(6):265-71. [View at Publisher] [DOI] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |