Wed, Nov 26, 2025
[Archive]
Volume 1, Issue 2 (10-2024)
IJHMD 2024, 1(2): 18-23 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Charkazi A, Rajabi A, Kazemi S B, Ahmadi-Livani M, Ozouni-Davaji R B. Anxiety, depression symptoms, and sleep quality in frontline health workers during COVID-19 pandemic in Northeast of Iran: A Cross-Sectional Study. IJHMD 2024; 1 (2) :18-23
URL: http://jhd.goums.ac.ir/article-1-32-en.html
URL: http://jhd.goums.ac.ir/article-1-32-en.html
Abdurrahman Charkazi1 

 , Abdolhalim Rajabi2
, Abdolhalim Rajabi2 

 , Sakineh Begum Kazemi2
, Sakineh Begum Kazemi2 
 , Maryam Ahmadi-Livani2
, Maryam Ahmadi-Livani2 

 , Rahman Berdi Ozouni-Davaji *3
, Rahman Berdi Ozouni-Davaji *3 




 , Abdolhalim Rajabi2
, Abdolhalim Rajabi2 

 , Sakineh Begum Kazemi2
, Sakineh Begum Kazemi2 
 , Maryam Ahmadi-Livani2
, Maryam Ahmadi-Livani2 

 , Rahman Berdi Ozouni-Davaji *3
, Rahman Berdi Ozouni-Davaji *3 


1- Environmental Health Research Center, Golestan University of Medical Sciences, Gorgan, Iran
2- Health Management and Social Development Research Center, Golestan University of Medical Sciences, Gorgan, Iran
3- Health Management and Social Development Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,davajirahman@gmail.com
2- Health Management and Social Development Research Center, Golestan University of Medical Sciences, Gorgan, Iran
3- Health Management and Social Development Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,
Full-Text [PDF 567 kb]
(496 Downloads)
| Abstract (HTML) (1955 Views)
Full-Text: (437 Views)
Introduction
In December 2019, there was an outbreak of an unknown pneumonia in Wuhan, Hubei Province, China, and caused serious concerns not only in China but also in the international arena (1). SARS-COV-2 virus induced this unknown corona pneumonia and has now spread in many countries. On January 30, 2020, the Emergency Committee of the World Health Organization declared this disease as a global health emergency due to its significant growth in China and other countries (2). The early symptoms of SARS-COV-2 are related to COVID-19 disease emerged with symptoms of pneumonia. Recent reports have documented gastrointestinal symptoms and asymptomatic infections in patients, especially children (3). The incubation period of this unknown disease is five days on average with the median of three days in a range of 0-24 days (4,5). In symptomatic patients, clinical manifestations such as fever, cough, nasal inflammation, fatigue, and other symptoms of upper respiratory tract infection usually appear over less than a week. Infection raises severe respiratory diseases and severe chest symptoms, which induce pneumonia in 75% of patients and are observed in CT scan images of the lungs at the admission time (4). One of the main features of SARS-COV-2 is its high infectivity. A recent study on 425 confirmed patients revealed that the number of patients in this epidemic is doubled per week, with each patient infecting an average of 2.2 persons (3). The analyses of recent findings from the early stages of the outbreak have also suggested that the infection rate ranges from 2.2 to 3.58 persons (6).
Because of the high speed and transmission power of this disease, some cases are also observed in Iran. The first case was reported on February 18, 2017 in Qom, and it was then spread across the country. According to Worldometers.info, 7739424 coronavirus cases with 428336 deaths and 3966208 recovered patients were reported worldwide by June 13, 2020. In Iran, 182525 cases, with 8659 deaths and 144649 recovered patients, have been reported. In this regard, Iran is globally ranked tenth, following the United States, Brazil, Russia, India, England, Spain, Italy, Peru, and Germany (7).
The rapid increase in the number of positive cases of this disease and relevant deaths have aroused psychological problems such as anxiety, depression, and stress among both medical staff and the general public (8). In other words, the prevalence of COVID-19 has not only raised a major public health concern but also posed high levels of psychological distress, especially among medical personnel (9). The findings of a study revealed that 67.2% of medical personnel on the frontline of the fight against COVID-19 disease suffered from sleep problems, and that such sleep problems were significantly more prevalent among women than men (5). According to the findings of another study, 36.1% of medical personnel involved in the fight against COVID -19 suffered from insomnia. More interestingly, the same study reported a relationship between insomnia with the level of education, profession, working in isolation ward, concerns about being infected, understanding the non-psychological support of news and social media during the COVID-19 outbreak, and low confidence to control the disease. In this regard, there have been reports on the prevalence of depression (50.7%), anxiety (44.7%), and symptom-relevant stress (73.4%) (9). Many studies have also documented different prevalence rates of psychological problems among the frontline personnel. In a study, there was a 38% increase in the prevalence of sleep problems among the medical staff. 5 Lai et al. reported the symptoms of depression (50.4%), anxiety (64.6%), insomnia (34%), and distress (71.5%) among the staff on the frontline of the fight against COVID-19 disease (10).
In Wuhan, China, a study on nurses and physicians revealed that 34.4%, 22.4%, and 6.2% of the participants had low, moderate, and severe mental health status (11). Another study in Gansu, China, reported that the prevalence rates of anxiety and depression were 11.4% and 45.6% in physicians and 27.9% and 43.0% in nurses, respectively (12). In Iran, few studies have addressed mental health problems among the frontline personnel fighting against COVID-19 disease. However, a study reported the prevalence rates of 51.4% and 52% for depression and 68.6% and 68.5% for anxiety among nurses and physicians, respectively (13). In another study, (14) 39.6% of hospital staff was suffering from moderate to severe anxiety, and women, nurses, and employees aged above 40 years experienced higher levels of anxiety. In this regard, psychological problems seem to be more prevalent in Iran, compared to other countries.
In their fight against COVID-19 disease, the medical staff in Wuhan were exposed to a lot of pressure posed by following factors: high risk of transmission, improper protection against infection, overwork, failure or despair, isolation, patients with negative emotions, lack of contact with their families, fatigue, exhaustion, and worn out. The tough conditions may arouse mental health problems such as stress, anxiety, symptoms of depression, insomnia, denial, anger, and fear, which affect not only medical staff’s attention and concentration but also their understanding and decision-making ability. This would consequently hinder appropriate fight against COVID-19 and have long-term impacts on their general well-being (8). Moreover, health professionals, especially the ones in hospitals who take care of patients with confirmed or suspected COVID-19 pneumonia, are at the high risk of disease transmission and psychological problems. They may be afraid of spreading and transmitting the virus to their families, friends, or colleagues. A study on health staff in Beijing Hospital revealed that those who were quarantined, were in a high-risk clinical ward, such as SARS ward, or had family members or friends with SARS, exhibited relatively more post-traumatic stress symptoms than the ones not having such experiences (15).
Protecting medical staff is of great importance to control their long-term illness and health epidemic (8) as such the detection of mental health responses following public health emergencies would make medical staff and communities be prepared and appropriately respond to disasters (16). However, little epidemiological data is available on mental health problems and psychiatric complications of individuals suspected or diagnosed with COVID-19 and health professionals involved in treatment processes. Accordingly, it is not crystal clear how to best respond to challenges during an outbreak (17). In a similar vein, the present study aimed to explore generalized anxiety disorder, sleep quality, and symptoms of depression, as well as factors affecting these variables among the medical personnel involved in the fight against COVID-19 disease in the hospitals in Northeast of Iran, 2020.
Methods
Study design
This cross-sectional study adopted a descriptive-analytical approach. The project (Ethics code: IR.GOUMS.REC.1399.003) was approved by the Ethics Committee of Golestan University of Medical Sciences and the ethics committee of Iran’s biomedical studies.
Sample
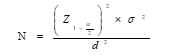
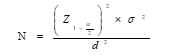
The study population encompassed all medical personnel involved in the fight against corona virus in hospitals in Golestan province, who were also the Telegram and WhatsApp group members. According to the existing information, the medical staffs involved in the fight against Coronavirus are about 5000 persons, among whom there are about 4000 nurses, midwives, and paramedics, about 750 doctors, and 20 service personnel. According to Jing Qi’s et al. (5) study in China and with regard to confidence level of 95% and the largest standard deviation for sleep disorder (4,3), the minimum sample size was estimated to be 385. The sample size was calculated using the following equation:
Since the study was carried out in cyberspace via social networks, the questionnaires were submitted to individuals who met the inclusion criteria. One of the university personnel appointed by the Vice Chancellor for Treatment sent and followed up the questionnaires to the social groups of each of the hospitals in Golestan province to ensure that the questionnaires were completed in all the hospitals involved in the fight against COVID-19 disease. The required data were collected during April and May, 2020.
Instrument
The assessment instrument was a questionnaire with four sections: (1) Demographic questions, (2) Short Form of Generalized Anxiety Disorder, (3) Sleep Quality Index, and (4) Patient Health Questionnaire.
1. Demographic questions: This section addressed the participants’ age, gender, level of education, background of employment, hospital, occupation, type of employment, place of residence (City or village), and city of residence.
2. Short Form of Generalized Anxiety Disorder: This questionnaire was developed by Spitzer, Kroenke, Williams, and Löwe (18) to diagnose generalized anxiety disorder and assess the severity of clinical symptoms. This questionnaire contained seven main questions and one additional question addressing the extent to which the disorder interferes with individuals’ performance. The total anxiety score is the sum of the seven questions, ranging from 0 to 21. A four-point Likert scale ranging from 0 to 3 is used to score this questionnaire; hence, the scoring scale consisted of never (0), sometimes (1), often (2), and almost always (3). The minimum and maximum scores were zero and 21, with higher scores indicating higher levels of anxiety. No reverse scoring was used for the items. In this study, we defined the anxiety score as 9, which was larger than the one set in this questionnaire. Cronbach's alpha coefficient was reported to be 0.92, and the test-retest coefficient with a two-week interval was also reported to be 0.83 (18). Naeinian, Shaeiri, Sharifi, and Hadian confirmed the questionnaire reliability using Cronbach's alpha coefficient and test-retest technique (19).
3. Pittsburgh Sleep Quality Index: This questionnaire was developed by Buysse et al. (1989) as a measure of sleep quality. The index is a self-report questionnaire that assesses sleep quality over a one-month time interval. It basically contains nine items; however, Item 5 itself encompasses 10 sub-items as such it consists of 19 items classified into seven components (Namely subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction). Each of the components is scored based on a 4-point Likert scale ranging from 0 to 3, with 3 indicating the highest malfunction. The scores of the components create a global score, and the total score ranges from zero to 21, with the higher scores representing lower sleep quality and the score ≤7 reflecting low sleep quality. The internal consistency of the questionnaire was reported to be 0.83 using Cronbach's alpha coefficient, reflecting high internal consistency (20). In Iran, the validity and reliability of this index were assessed by Farahi Moghadam et al. as they reported its internal consistency to be 0.77 using Cronbach's alpha coefficient. Furthermore, the correlation between sleep quality and general health questionnaire was also reported to be 0.54 (21).
4. Patient Health Questionnaire (PHQ-9): the PHQ-9 is a nine-item self-reported questionnaire to assess the presence of depression symptoms over a two-week time interval (22). The questionnaire scores range from 0 (No symptom of depression) to 27 (Severe symptoms of depression). This questionnaire was scored using a four-point Likert scale ranging from 0 to 3: never (0), sometimes (1), often (2), and almost always (3). The minimum and maximum scores were zero and 27, and there was no reverse scoring for the items. The validity and reliability of the above questionnaire have been reported to be high (22). The reliability of the Persian version of this questionnaire was reported to be 0.88 using Cronbach's alpha coefficient and 0.79 after a two-week interval (23). In this study, scores ≥10 were considered as the presence of the depression symptoms.
Data collection
The questionnaires were developed electronically and sent to different medical staff groups. Inclusion criteria consisted of being a hospital staff, having smartphones with installed social networks applications, and being willing to participate.
Data analysis
The collected data were imported to STATA statistical software version 12. Quantitative and qualitative data were presented using descriptive statistics (Namely mean, standard deviation, percentage, and frequency), respectively. Moreover, univariate and multivariate logistic regression analyses were used to examine the impacts of the measured variables on anxiety, symptoms of depression, and low sleep quality. In this study, the significance level was considered to be <0.05.
Ethical considerations
The Ethical Review Committee of Golestan University of Medical Sciences and the Ethics committee of Iran’s Biomedical Studies approved the study (Ethics code: IR.GOUMS.REC.1399.003). The study objectives were explained to all participants and they were assured their personal data and responses would be kept confidential.
Results
The data collected from 580 medical staff were analyzed in this study. Among the participants, there were175 males (30.17%), and the participants’ mean age was 35.72 ± 8.39 years. Moreover, there were 341 nurses (58.79%), and 285 persons (49.14%) had a work experience of ≥10 years. Table 1 presents the other demographic characteristics of the study participants.
Table 2 shows the prevalence of anxiety, symptoms of depression and sleep quality among the participants by gender. In general, the prevalence rates of anxiety, symptoms of depression, and sleep quality were 50.52%, 28.10%, and 71.03%, respectively. As it can be observed, no significant difference is noticed between men and women in terms of depression symptoms and sleep quality; however, the level of anxiety is significantly higher in women than men (P = 0.002).
No significant difference was also detected regarding the prevalence rates of anxiety and symptoms of depression at the age ranges of <35 years and > 35 years. On the other hand, 76.36% of the participants at the age range of >35 years had significantly low sleep quality (p = 0.007) (Table 3).
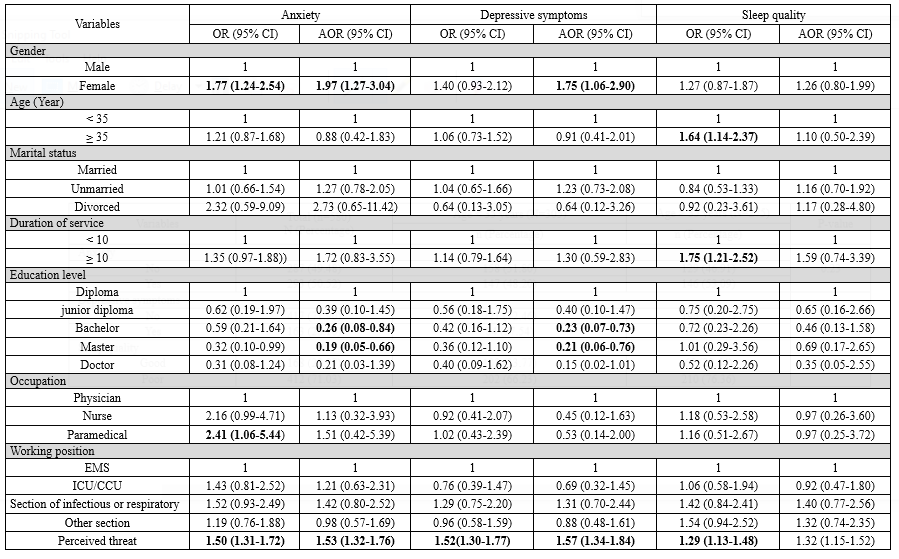
Table 4 shows the relationship between potential factors of anxiety, symptoms of depression, and sleep quality during the COVID-19 epidemic. According to the results of the univariate analysis, females in comparison to males (OR = 1.77, 95% CI: 1.24-2.54), paramedical occupations in comparison to physicians (OR = 2.41, 95% CI: 1.06-5.44), and high perceived threat (OR = 1.50, 95% CI: 1.31-1.72) were significantly correlated with increased anxiety. Unlike anxiety, the symptoms of depression exhibited a significant correlation with high perceived threat (1.52, 95% CI: 1.30-1.77 OR =). Moreover, significant correlations were also detected between sleep quality and the age range of > 35 years (1.64, 95% CI: 1.14-2.37 OR =), work experience of >10 years (OR = 1.75, 95% CI: 1.21-2.52), and high perceived threat (OR = 1.29, 95 % CI: 1.13-1.48).
In the multivariate logistic regression analysis, the relationships between gender and high perceived threat with anxiety were still significant; however, no significant relationship was observed between paramedical occupations and anxiety (OR = 1.51, 95% CI: 0.42- 5.39). Regarding the level of education in this model, in comparison to diploma, holding a bachelor's degree (OR = 0.26, 95% CI: 0.08-0.84) and a master's degree (OR = 0.19, 95% CI: 0.05-0) decreased the likelihood of anxiety. The same relationships were also observed for symptoms of depression. Unlike anxiety and symptoms of depression in the multivariate model, no significant relationship was observed between potential variables and the participants' sleep quality.
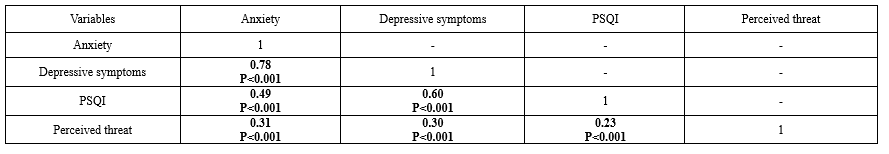
Correlation analysis was conducted to examine the correlations between anxiety, depressive symptoms, sleep quality, and perceived threat (Table 5), according to which anxiety was significantly correlated with symptoms of depression (r = 0.78, p <0.001), sleep quality (r = 0.49, p <0.001), and perceived threat (r = 0.31, p <0.001).
In December 2019, there was an outbreak of an unknown pneumonia in Wuhan, Hubei Province, China, and caused serious concerns not only in China but also in the international arena (1). SARS-COV-2 virus induced this unknown corona pneumonia and has now spread in many countries. On January 30, 2020, the Emergency Committee of the World Health Organization declared this disease as a global health emergency due to its significant growth in China and other countries (2). The early symptoms of SARS-COV-2 are related to COVID-19 disease emerged with symptoms of pneumonia. Recent reports have documented gastrointestinal symptoms and asymptomatic infections in patients, especially children (3). The incubation period of this unknown disease is five days on average with the median of three days in a range of 0-24 days (4,5). In symptomatic patients, clinical manifestations such as fever, cough, nasal inflammation, fatigue, and other symptoms of upper respiratory tract infection usually appear over less than a week. Infection raises severe respiratory diseases and severe chest symptoms, which induce pneumonia in 75% of patients and are observed in CT scan images of the lungs at the admission time (4). One of the main features of SARS-COV-2 is its high infectivity. A recent study on 425 confirmed patients revealed that the number of patients in this epidemic is doubled per week, with each patient infecting an average of 2.2 persons (3). The analyses of recent findings from the early stages of the outbreak have also suggested that the infection rate ranges from 2.2 to 3.58 persons (6).
Because of the high speed and transmission power of this disease, some cases are also observed in Iran. The first case was reported on February 18, 2017 in Qom, and it was then spread across the country. According to Worldometers.info, 7739424 coronavirus cases with 428336 deaths and 3966208 recovered patients were reported worldwide by June 13, 2020. In Iran, 182525 cases, with 8659 deaths and 144649 recovered patients, have been reported. In this regard, Iran is globally ranked tenth, following the United States, Brazil, Russia, India, England, Spain, Italy, Peru, and Germany (7).
The rapid increase in the number of positive cases of this disease and relevant deaths have aroused psychological problems such as anxiety, depression, and stress among both medical staff and the general public (8). In other words, the prevalence of COVID-19 has not only raised a major public health concern but also posed high levels of psychological distress, especially among medical personnel (9). The findings of a study revealed that 67.2% of medical personnel on the frontline of the fight against COVID-19 disease suffered from sleep problems, and that such sleep problems were significantly more prevalent among women than men (5). According to the findings of another study, 36.1% of medical personnel involved in the fight against COVID -19 suffered from insomnia. More interestingly, the same study reported a relationship between insomnia with the level of education, profession, working in isolation ward, concerns about being infected, understanding the non-psychological support of news and social media during the COVID-19 outbreak, and low confidence to control the disease. In this regard, there have been reports on the prevalence of depression (50.7%), anxiety (44.7%), and symptom-relevant stress (73.4%) (9). Many studies have also documented different prevalence rates of psychological problems among the frontline personnel. In a study, there was a 38% increase in the prevalence of sleep problems among the medical staff. 5 Lai et al. reported the symptoms of depression (50.4%), anxiety (64.6%), insomnia (34%), and distress (71.5%) among the staff on the frontline of the fight against COVID-19 disease (10).
In Wuhan, China, a study on nurses and physicians revealed that 34.4%, 22.4%, and 6.2% of the participants had low, moderate, and severe mental health status (11). Another study in Gansu, China, reported that the prevalence rates of anxiety and depression were 11.4% and 45.6% in physicians and 27.9% and 43.0% in nurses, respectively (12). In Iran, few studies have addressed mental health problems among the frontline personnel fighting against COVID-19 disease. However, a study reported the prevalence rates of 51.4% and 52% for depression and 68.6% and 68.5% for anxiety among nurses and physicians, respectively (13). In another study, (14) 39.6% of hospital staff was suffering from moderate to severe anxiety, and women, nurses, and employees aged above 40 years experienced higher levels of anxiety. In this regard, psychological problems seem to be more prevalent in Iran, compared to other countries.
In their fight against COVID-19 disease, the medical staff in Wuhan were exposed to a lot of pressure posed by following factors: high risk of transmission, improper protection against infection, overwork, failure or despair, isolation, patients with negative emotions, lack of contact with their families, fatigue, exhaustion, and worn out. The tough conditions may arouse mental health problems such as stress, anxiety, symptoms of depression, insomnia, denial, anger, and fear, which affect not only medical staff’s attention and concentration but also their understanding and decision-making ability. This would consequently hinder appropriate fight against COVID-19 and have long-term impacts on their general well-being (8). Moreover, health professionals, especially the ones in hospitals who take care of patients with confirmed or suspected COVID-19 pneumonia, are at the high risk of disease transmission and psychological problems. They may be afraid of spreading and transmitting the virus to their families, friends, or colleagues. A study on health staff in Beijing Hospital revealed that those who were quarantined, were in a high-risk clinical ward, such as SARS ward, or had family members or friends with SARS, exhibited relatively more post-traumatic stress symptoms than the ones not having such experiences (15).
Protecting medical staff is of great importance to control their long-term illness and health epidemic (8) as such the detection of mental health responses following public health emergencies would make medical staff and communities be prepared and appropriately respond to disasters (16). However, little epidemiological data is available on mental health problems and psychiatric complications of individuals suspected or diagnosed with COVID-19 and health professionals involved in treatment processes. Accordingly, it is not crystal clear how to best respond to challenges during an outbreak (17). In a similar vein, the present study aimed to explore generalized anxiety disorder, sleep quality, and symptoms of depression, as well as factors affecting these variables among the medical personnel involved in the fight against COVID-19 disease in the hospitals in Northeast of Iran, 2020.
Methods
Study design
This cross-sectional study adopted a descriptive-analytical approach. The project (Ethics code: IR.GOUMS.REC.1399.003) was approved by the Ethics Committee of Golestan University of Medical Sciences and the ethics committee of Iran’s biomedical studies.
Sample
The study population encompassed all medical personnel involved in the fight against corona virus in hospitals in Golestan province, who were also the Telegram and WhatsApp group members. According to the existing information, the medical staffs involved in the fight against Coronavirus are about 5000 persons, among whom there are about 4000 nurses, midwives, and paramedics, about 750 doctors, and 20 service personnel. According to Jing Qi’s et al. (5) study in China and with regard to confidence level of 95% and the largest standard deviation for sleep disorder (4,3), the minimum sample size was estimated to be 385. The sample size was calculated using the following equation:
Since the study was carried out in cyberspace via social networks, the questionnaires were submitted to individuals who met the inclusion criteria. One of the university personnel appointed by the Vice Chancellor for Treatment sent and followed up the questionnaires to the social groups of each of the hospitals in Golestan province to ensure that the questionnaires were completed in all the hospitals involved in the fight against COVID-19 disease. The required data were collected during April and May, 2020.
Instrument
The assessment instrument was a questionnaire with four sections: (1) Demographic questions, (2) Short Form of Generalized Anxiety Disorder, (3) Sleep Quality Index, and (4) Patient Health Questionnaire.
1. Demographic questions: This section addressed the participants’ age, gender, level of education, background of employment, hospital, occupation, type of employment, place of residence (City or village), and city of residence.
2. Short Form of Generalized Anxiety Disorder: This questionnaire was developed by Spitzer, Kroenke, Williams, and Löwe (18) to diagnose generalized anxiety disorder and assess the severity of clinical symptoms. This questionnaire contained seven main questions and one additional question addressing the extent to which the disorder interferes with individuals’ performance. The total anxiety score is the sum of the seven questions, ranging from 0 to 21. A four-point Likert scale ranging from 0 to 3 is used to score this questionnaire; hence, the scoring scale consisted of never (0), sometimes (1), often (2), and almost always (3). The minimum and maximum scores were zero and 21, with higher scores indicating higher levels of anxiety. No reverse scoring was used for the items. In this study, we defined the anxiety score as 9, which was larger than the one set in this questionnaire. Cronbach's alpha coefficient was reported to be 0.92, and the test-retest coefficient with a two-week interval was also reported to be 0.83 (18). Naeinian, Shaeiri, Sharifi, and Hadian confirmed the questionnaire reliability using Cronbach's alpha coefficient and test-retest technique (19).
3. Pittsburgh Sleep Quality Index: This questionnaire was developed by Buysse et al. (1989) as a measure of sleep quality. The index is a self-report questionnaire that assesses sleep quality over a one-month time interval. It basically contains nine items; however, Item 5 itself encompasses 10 sub-items as such it consists of 19 items classified into seven components (Namely subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction). Each of the components is scored based on a 4-point Likert scale ranging from 0 to 3, with 3 indicating the highest malfunction. The scores of the components create a global score, and the total score ranges from zero to 21, with the higher scores representing lower sleep quality and the score ≤7 reflecting low sleep quality. The internal consistency of the questionnaire was reported to be 0.83 using Cronbach's alpha coefficient, reflecting high internal consistency (20). In Iran, the validity and reliability of this index were assessed by Farahi Moghadam et al. as they reported its internal consistency to be 0.77 using Cronbach's alpha coefficient. Furthermore, the correlation between sleep quality and general health questionnaire was also reported to be 0.54 (21).
4. Patient Health Questionnaire (PHQ-9): the PHQ-9 is a nine-item self-reported questionnaire to assess the presence of depression symptoms over a two-week time interval (22). The questionnaire scores range from 0 (No symptom of depression) to 27 (Severe symptoms of depression). This questionnaire was scored using a four-point Likert scale ranging from 0 to 3: never (0), sometimes (1), often (2), and almost always (3). The minimum and maximum scores were zero and 27, and there was no reverse scoring for the items. The validity and reliability of the above questionnaire have been reported to be high (22). The reliability of the Persian version of this questionnaire was reported to be 0.88 using Cronbach's alpha coefficient and 0.79 after a two-week interval (23). In this study, scores ≥10 were considered as the presence of the depression symptoms.
Data collection
The questionnaires were developed electronically and sent to different medical staff groups. Inclusion criteria consisted of being a hospital staff, having smartphones with installed social networks applications, and being willing to participate.
Data analysis
The collected data were imported to STATA statistical software version 12. Quantitative and qualitative data were presented using descriptive statistics (Namely mean, standard deviation, percentage, and frequency), respectively. Moreover, univariate and multivariate logistic regression analyses were used to examine the impacts of the measured variables on anxiety, symptoms of depression, and low sleep quality. In this study, the significance level was considered to be <0.05.
Ethical considerations
The Ethical Review Committee of Golestan University of Medical Sciences and the Ethics committee of Iran’s Biomedical Studies approved the study (Ethics code: IR.GOUMS.REC.1399.003). The study objectives were explained to all participants and they were assured their personal data and responses would be kept confidential.
Results
The data collected from 580 medical staff were analyzed in this study. Among the participants, there were175 males (30.17%), and the participants’ mean age was 35.72 ± 8.39 years. Moreover, there were 341 nurses (58.79%), and 285 persons (49.14%) had a work experience of ≥10 years. Table 1 presents the other demographic characteristics of the study participants.
Table 2 shows the prevalence of anxiety, symptoms of depression and sleep quality among the participants by gender. In general, the prevalence rates of anxiety, symptoms of depression, and sleep quality were 50.52%, 28.10%, and 71.03%, respectively. As it can be observed, no significant difference is noticed between men and women in terms of depression symptoms and sleep quality; however, the level of anxiety is significantly higher in women than men (P = 0.002).
No significant difference was also detected regarding the prevalence rates of anxiety and symptoms of depression at the age ranges of <35 years and > 35 years. On the other hand, 76.36% of the participants at the age range of >35 years had significantly low sleep quality (p = 0.007) (Table 3).
Table 4 shows the relationship between potential factors of anxiety, symptoms of depression, and sleep quality during the COVID-19 epidemic. According to the results of the univariate analysis, females in comparison to males (OR = 1.77, 95% CI: 1.24-2.54), paramedical occupations in comparison to physicians (OR = 2.41, 95% CI: 1.06-5.44), and high perceived threat (OR = 1.50, 95% CI: 1.31-1.72) were significantly correlated with increased anxiety. Unlike anxiety, the symptoms of depression exhibited a significant correlation with high perceived threat (1.52, 95% CI: 1.30-1.77 OR =). Moreover, significant correlations were also detected between sleep quality and the age range of > 35 years (1.64, 95% CI: 1.14-2.37 OR =), work experience of >10 years (OR = 1.75, 95% CI: 1.21-2.52), and high perceived threat (OR = 1.29, 95 % CI: 1.13-1.48).
In the multivariate logistic regression analysis, the relationships between gender and high perceived threat with anxiety were still significant; however, no significant relationship was observed between paramedical occupations and anxiety (OR = 1.51, 95% CI: 0.42- 5.39). Regarding the level of education in this model, in comparison to diploma, holding a bachelor's degree (OR = 0.26, 95% CI: 0.08-0.84) and a master's degree (OR = 0.19, 95% CI: 0.05-0) decreased the likelihood of anxiety. The same relationships were also observed for symptoms of depression. Unlike anxiety and symptoms of depression in the multivariate model, no significant relationship was observed between potential variables and the participants' sleep quality.
Correlation analysis was conducted to examine the correlations between anxiety, depressive symptoms, sleep quality, and perceived threat (Table 5), according to which anxiety was significantly correlated with symptoms of depression (r = 0.78, p <0.001), sleep quality (r = 0.49, p <0.001), and perceived threat (r = 0.31, p <0.001).
|
Table 1. Demographic characteristics of study sample (N=580)
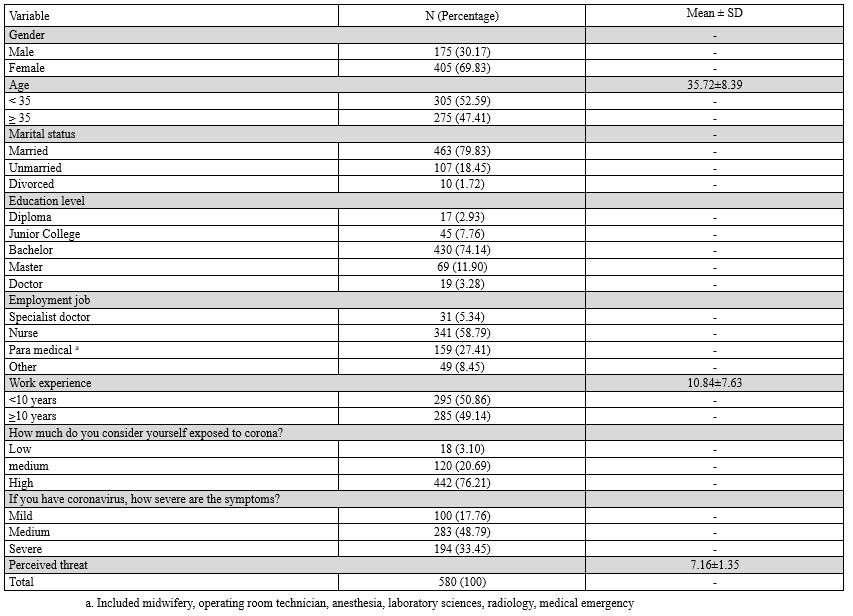 Table 2. Prevalence of anxiety, depressive symptoms, and sleep quality during COVID-19 epidemic in Iran population stratified by gender (N=580) 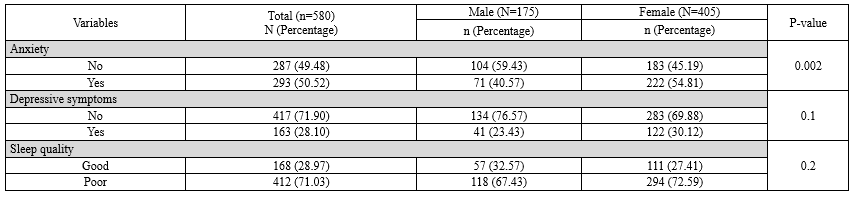 Table 3. Prevalence of anxiety, depressive symptoms, and sleep quality during COVID-19 epidemic in Iran population stratified by age group (N=580)  |
Moreover, a significant direct relationship between symptoms of depression with sleep quality (r = 0.60, p <0.001) and perceived threat (r = 0.30, p <0.001). Further, a significant direct relationship was observed between perceived threat and sleep quality (r = 0.23, p <0.001) (Table 5).
Discussion
This study aimed to examine the prevalence of anxiety, symptoms of depression, and sleep quality, as well as the factors affecting these variables among the frontline hospital personnel involved in the fight against COVID-19 in Golestan Province, Iran. In this regard, the study findings revealed that the most common psychological problems were low sleep quality (71.03%), anxiety (50.5%), and depression symptoms (28.10%) among the concerned personnel.
The findings of this study are in line with those of Wang’s et al. (5) study on sleep problems as they revealed that 67.2% of medical workers on the frontline of the fight against COVID-19 had sleep problems and that women had more sleep problems than men. In another study, Zhang et al. (9) reported that 36.1% of medical staff involved in the fight against COVID -19 had insomnia. Moreover, the prevalence rates of sleep problems in medical personnel were 38% in Wang’s et al. study (5) and 34% in Lai’s et al. (10)
Additionally, another finding of this study indicated the anxiety rate of 50.52 in medical staff on the frontline of the fight against COVID-19. The reported value was larger than the value (11.4%) reported by Zhu et al. (12) and the one reported by Kaveh et al, (14) who revealed that 39.6% of hospital staff experienced moderate to severe anxiety. In Kaveh’s et al. (14) study there were higher levels of anxiety in women aged > 40 years and nurses. The reported prevalence rate of anxiety in this study was smaller than the rates reported by Hassannia et al. (13) among nurses (68.6%) and physicians (68.5%).
In general, the level of anxiety and sleep problems in Iranian healthcare personnel seem to be higher than the other countries. This can be due to the problem with having access to personal protective equipment to take care of oneself and patients. Strict sanctions have been imposed on Iran, which have limited access to medical equipment. Iran's health system is the most resilient health system across the region; however, it has been affected by sanctions. This would in turn directly and indirectly influence all prevention, diagnosis, and treatment measures. Lack of medical, pharmaceutical, and laboratory equipment such as protective gowns and essential medicines and drugs has enhanced the burden of this epidemics and the number of casualties (24). This would enhance anxiety and in turn reduce sleep quality and raise sleep problems.
In this study, another factor arousing anxiety and sleep problems is the fear of transmitting the virus to family members regarding the highly contagious nature of the concerned virus (3,6). The tough conditions may arouse mental health problems such as stress, anxiety, symptoms of depression, insomnia, denial, anger, and fear, which affect not only medical staff’s attention and concentration but also their understanding and decision-making ability. This would in turn hinder appropriate fight against COVID-19 and have long-term impacts on their general well-being (8). Moreover, health professionals, especially the ones in hospitals who take care of patients with confirmed or suspected COVID-19 pneumonia, are at the high risk of disease transmission and psychological problems. They may be afraid of spreading and transmitting the virus to their families, friends, or colleagues. A study on health staff in Beijing Hospital revealed that those who were quarantined, were in a high-risk clinical ward, such as SARS ward, or had family members or friends with SARS, exhibited relatively more post-traumatic stress symptoms than the ones having not such experiences (15).
Finally, the present study also revealed that 28 percent of the samples suffered from depression symptoms. This finding is in line with the findings in studies by Pappa et al. (25) reporting a 22.8% prevalence rate of depression symptoms in healthcare staff, Zhu et al. (12) reporting that 45.6% of physicians and 43.0% of nurses had symptoms of depression, and Hassannia et al (13). Suggesting that 51.4% of nurses and 52% of physicians had symptoms of depression. All these studies, but Pappa’s et al., reported higher prevalence rates of depression symptoms. In this regard, one of the factors leading to inconsistencies in the findings might be the research instruments used to examine the depression symptoms and the concerned cut-off point in these studies.
Another finding of this study suggested a significant relationship between perceived threats with anxiety, symptoms of depression, and sleep quality. Operationally, perceived threat is a combination of perceived sensitivity and perceived severity of a disease. Accordingly, individuals perceive themselves as susceptible to COVID-19 and strongly perceive the disease severity and complications at the same time. In other words, the medical staffs on the frontline of the fight against this disease perceive themselves to be at risk of the disease and believe in more severe and more fatal clinical symptoms and complications in the case of being infected. The perceived threat might have been caused by the fact that they are dealing with the patients every day and have witnessed severe symptoms in the patients and their deaths. This acts as a guide to external action, leading to the perceived severity of this disease. On the other hand, the lack of definite vaccines and treatments for this disease as well as its unknown nature can aggravate such feelings of fear and threat, resulting in enhanced levels of anxiety and depression accompanied with sleep disorders and reduced sleep quality. According to Li et al., high perceived severity increases negative emotions, cell phone use, and caution in the case of COVID-19 disease (26). Moreover, in their study conducted in the early stages of COVID-19 disease in Hong Kong, Kwok et al. revealed high perceived sensitivity and severity among the participants (27).
The other findings of the present study showed that the high perceived threat in females, compared to males, was significantly associated with increased levels of anxiety. Shahnazi et al. also found out that the preventive behaviors against COVID-19 disease were significantly more frequent among women than men (28). This is probably because of women’s stronger desire to be healthier, in comparison to men. Paramedics are also exposed to a higher perceived threat, in comparison to physicians, as they perceive themselves to be more likely to develop COVID-19 disease due to their frequent contacts with patients and continuous care. Unlike anxiety, only symptoms of depression were significantly correlated with high perceived threats. Sleep quality was significantly correlated with age range of >35 years, work experience of >10 years, and high perceived threats. In the multivariate logistic regression analysis, there was still a significant relationship between gender and the perceived high threat with anxiety; however, no significant relationship was observed between paramedical occupations and anxiety. According to this model, holding a bachelor's and master's degree, in comparison to diploma, reduced the likelihood of anxiety. Similar relationships are also observed for the symptoms of depression. Unlike anxiety and symptoms of depression, the multivariate model showed no significant relationship between potential variables with participants' sleep quality. An examination of the relationships between anxiety, symptoms of depression, sleep quality, and a perceived threat documented that anxiety was significantly and directly correlated with symptoms of depression, sleep quality, and perceived threat. Moreover, a significant direct relationship was found between depressive symptoms, sleep quality, and perceived threat. Additionally, a direct and significantly moderate relationship existed between perceived threat and sleep quality. Since the high perceived threat and fear of COVID-19 disease raised anxiety among the involved medical personnel, it also led to depression and sleep disorders.
Conclusion
The prevalence of COVID-19 has not only raised a major public health concern but also posed high levels of psychological distress, especially among medical personnel. In our study, 71.03% of frontline health workers during COVID-19 Pandemic in Iran suffered from low sleep quality, 50.5% had anxiety, and 28.10% had depression symptoms. There was a statistically significant relationship between perceived threats with anxiety, symptoms of depression, and sleep quality. The other findings of the present study showed that the high perceived threat in females, compared to males, was significantly associated with increased levels of anxiety. These findings provide planners, policymakers, and mental health professionals with valuable information about the psychological effects of the viral disease spread. The mental health problems of the personnel involved in the fight against COVID-19 disease should be researched and screened sooner to be provided with health services. On the other hand, training the health staff on how to deal with and manage themselves in such conditions psychologically would be effective in preventing psychological problems. Telemedicine can protect medical personnel, especially physicians as it enables staff to quarantine the ones exposed to COVID-19 disease at home and communicate with patients via a computer. This in turn reduces workload and optimizes the presence of patients with unfavorable conditions (29).
The present study also had some limitations. First, this cross-sectional study used self-report instruments, and this makes problems in detecting the causal relationships. However, logistic regression analysis was also employed. Second, the research samples consisted of individuals who were the members of social networks and excluded other individuals. This makes the generalization of the findings difficult.
Acknowledgement
The authors express their gratitude to all the individuals who participated in the study.
Funding sources
This study was approved and financially supported by the Golestan University of Medical Sciences. The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Ethical statement
The Ethics Committee of the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran, approved this study (Code: IR.GOUMS.REC.1399.003).
Conflicts of interest
The authors declared that they have no competing interests.
Author contributions
RBOD and AC contributed in designing the study. SBK and MAL collected the data, which was then analyzed by AR. The final report and article were written by RBOD and AC and RA. All authors have read and approved the manuscript.
Discussion
This study aimed to examine the prevalence of anxiety, symptoms of depression, and sleep quality, as well as the factors affecting these variables among the frontline hospital personnel involved in the fight against COVID-19 in Golestan Province, Iran. In this regard, the study findings revealed that the most common psychological problems were low sleep quality (71.03%), anxiety (50.5%), and depression symptoms (28.10%) among the concerned personnel.
The findings of this study are in line with those of Wang’s et al. (5) study on sleep problems as they revealed that 67.2% of medical workers on the frontline of the fight against COVID-19 had sleep problems and that women had more sleep problems than men. In another study, Zhang et al. (9) reported that 36.1% of medical staff involved in the fight against COVID -19 had insomnia. Moreover, the prevalence rates of sleep problems in medical personnel were 38% in Wang’s et al. study (5) and 34% in Lai’s et al. (10)
Additionally, another finding of this study indicated the anxiety rate of 50.52 in medical staff on the frontline of the fight against COVID-19. The reported value was larger than the value (11.4%) reported by Zhu et al. (12) and the one reported by Kaveh et al, (14) who revealed that 39.6% of hospital staff experienced moderate to severe anxiety. In Kaveh’s et al. (14) study there were higher levels of anxiety in women aged > 40 years and nurses. The reported prevalence rate of anxiety in this study was smaller than the rates reported by Hassannia et al. (13) among nurses (68.6%) and physicians (68.5%).
In general, the level of anxiety and sleep problems in Iranian healthcare personnel seem to be higher than the other countries. This can be due to the problem with having access to personal protective equipment to take care of oneself and patients. Strict sanctions have been imposed on Iran, which have limited access to medical equipment. Iran's health system is the most resilient health system across the region; however, it has been affected by sanctions. This would in turn directly and indirectly influence all prevention, diagnosis, and treatment measures. Lack of medical, pharmaceutical, and laboratory equipment such as protective gowns and essential medicines and drugs has enhanced the burden of this epidemics and the number of casualties (24). This would enhance anxiety and in turn reduce sleep quality and raise sleep problems.
In this study, another factor arousing anxiety and sleep problems is the fear of transmitting the virus to family members regarding the highly contagious nature of the concerned virus (3,6). The tough conditions may arouse mental health problems such as stress, anxiety, symptoms of depression, insomnia, denial, anger, and fear, which affect not only medical staff’s attention and concentration but also their understanding and decision-making ability. This would in turn hinder appropriate fight against COVID-19 and have long-term impacts on their general well-being (8). Moreover, health professionals, especially the ones in hospitals who take care of patients with confirmed or suspected COVID-19 pneumonia, are at the high risk of disease transmission and psychological problems. They may be afraid of spreading and transmitting the virus to their families, friends, or colleagues. A study on health staff in Beijing Hospital revealed that those who were quarantined, were in a high-risk clinical ward, such as SARS ward, or had family members or friends with SARS, exhibited relatively more post-traumatic stress symptoms than the ones having not such experiences (15).
Finally, the present study also revealed that 28 percent of the samples suffered from depression symptoms. This finding is in line with the findings in studies by Pappa et al. (25) reporting a 22.8% prevalence rate of depression symptoms in healthcare staff, Zhu et al. (12) reporting that 45.6% of physicians and 43.0% of nurses had symptoms of depression, and Hassannia et al (13). Suggesting that 51.4% of nurses and 52% of physicians had symptoms of depression. All these studies, but Pappa’s et al., reported higher prevalence rates of depression symptoms. In this regard, one of the factors leading to inconsistencies in the findings might be the research instruments used to examine the depression symptoms and the concerned cut-off point in these studies.
Another finding of this study suggested a significant relationship between perceived threats with anxiety, symptoms of depression, and sleep quality. Operationally, perceived threat is a combination of perceived sensitivity and perceived severity of a disease. Accordingly, individuals perceive themselves as susceptible to COVID-19 and strongly perceive the disease severity and complications at the same time. In other words, the medical staffs on the frontline of the fight against this disease perceive themselves to be at risk of the disease and believe in more severe and more fatal clinical symptoms and complications in the case of being infected. The perceived threat might have been caused by the fact that they are dealing with the patients every day and have witnessed severe symptoms in the patients and their deaths. This acts as a guide to external action, leading to the perceived severity of this disease. On the other hand, the lack of definite vaccines and treatments for this disease as well as its unknown nature can aggravate such feelings of fear and threat, resulting in enhanced levels of anxiety and depression accompanied with sleep disorders and reduced sleep quality. According to Li et al., high perceived severity increases negative emotions, cell phone use, and caution in the case of COVID-19 disease (26). Moreover, in their study conducted in the early stages of COVID-19 disease in Hong Kong, Kwok et al. revealed high perceived sensitivity and severity among the participants (27).
The other findings of the present study showed that the high perceived threat in females, compared to males, was significantly associated with increased levels of anxiety. Shahnazi et al. also found out that the preventive behaviors against COVID-19 disease were significantly more frequent among women than men (28). This is probably because of women’s stronger desire to be healthier, in comparison to men. Paramedics are also exposed to a higher perceived threat, in comparison to physicians, as they perceive themselves to be more likely to develop COVID-19 disease due to their frequent contacts with patients and continuous care. Unlike anxiety, only symptoms of depression were significantly correlated with high perceived threats. Sleep quality was significantly correlated with age range of >35 years, work experience of >10 years, and high perceived threats. In the multivariate logistic regression analysis, there was still a significant relationship between gender and the perceived high threat with anxiety; however, no significant relationship was observed between paramedical occupations and anxiety. According to this model, holding a bachelor's and master's degree, in comparison to diploma, reduced the likelihood of anxiety. Similar relationships are also observed for the symptoms of depression. Unlike anxiety and symptoms of depression, the multivariate model showed no significant relationship between potential variables with participants' sleep quality. An examination of the relationships between anxiety, symptoms of depression, sleep quality, and a perceived threat documented that anxiety was significantly and directly correlated with symptoms of depression, sleep quality, and perceived threat. Moreover, a significant direct relationship was found between depressive symptoms, sleep quality, and perceived threat. Additionally, a direct and significantly moderate relationship existed between perceived threat and sleep quality. Since the high perceived threat and fear of COVID-19 disease raised anxiety among the involved medical personnel, it also led to depression and sleep disorders.
Conclusion
The prevalence of COVID-19 has not only raised a major public health concern but also posed high levels of psychological distress, especially among medical personnel. In our study, 71.03% of frontline health workers during COVID-19 Pandemic in Iran suffered from low sleep quality, 50.5% had anxiety, and 28.10% had depression symptoms. There was a statistically significant relationship between perceived threats with anxiety, symptoms of depression, and sleep quality. The other findings of the present study showed that the high perceived threat in females, compared to males, was significantly associated with increased levels of anxiety. These findings provide planners, policymakers, and mental health professionals with valuable information about the psychological effects of the viral disease spread. The mental health problems of the personnel involved in the fight against COVID-19 disease should be researched and screened sooner to be provided with health services. On the other hand, training the health staff on how to deal with and manage themselves in such conditions psychologically would be effective in preventing psychological problems. Telemedicine can protect medical personnel, especially physicians as it enables staff to quarantine the ones exposed to COVID-19 disease at home and communicate with patients via a computer. This in turn reduces workload and optimizes the presence of patients with unfavorable conditions (29).
The present study also had some limitations. First, this cross-sectional study used self-report instruments, and this makes problems in detecting the causal relationships. However, logistic regression analysis was also employed. Second, the research samples consisted of individuals who were the members of social networks and excluded other individuals. This makes the generalization of the findings difficult.
Acknowledgement
The authors express their gratitude to all the individuals who participated in the study.
Funding sources
This study was approved and financially supported by the Golestan University of Medical Sciences. The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Ethical statement
The Ethics Committee of the University of Social Welfare and Rehabilitation Sciences, Tehran, Iran, approved this study (Code: IR.GOUMS.REC.1399.003).
Conflicts of interest
The authors declared that they have no competing interests.
Author contributions
RBOD and AC contributed in designing the study. SBK and MAL collected the data, which was then analyzed by AR. The final report and article were written by RBOD and AC and RA. All authors have read and approved the manuscript.
Type of Study: Original Article |
Subject:
Clinical
Received: 2023/12/24 | Accepted: 2024/11/20 | Published: 2024/12/10
Received: 2023/12/24 | Accepted: 2024/11/20 | Published: 2024/12/10
References
1. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470-3. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Velavan TP, Meyer CG. The COVID‐19 epidemic. Trop Med Int Health. 2020;25(3):278-80. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Chan JF-W, Yuan S, Kok K-H, To KK-W, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514-23. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Guan W-j, Ni Z-y, H-u Y, Liang W-h, Ou C-q, He J-x, et al. Clinical characteristics of 2019 novel coronavirus infection in China. MedRxiv. 2020. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occupational Medicine. 2020;70(5):364-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Zhao S, Lin Q, Ran J, Musa SS, Yang G, Wang W, et al. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: A data-driven analysis in the early phase of the outbreak. Int J Infect Dis. 2020;92:214-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. OUTBREAK C-C. Coronavirus Cases. 2020. [View at Publisher]
8. Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7(3):e14. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. 2020;11:306. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav Immun. 2020;87:11-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Zhu J, Sun L, Zhang L, Wang H, Fan A, Yang B, et al. Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu. Front Psychiatry. 2020;11:386. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Hassannia L, Taghizadeh F, Moosazadeh M, Zarghami M, Taghizadeh H, Dooki AF, et al. Anxiety and Depression in Health Workers and General Population During COVID-19 Epidemic in IRAN: A Web-Based Cross-Sectional Study. medRxiv. 2020. [View at Publisher] [DOI] [Google Scholar]
14. Kaveh M, Davari-tanha F, Varaei S, Shirali E, Shokouhi N, Nazemi P, et al. Anxiety levels among Iranian health care workers during the COVID-19 surge: A cross-sectional study. MedRxiv. 2020. [View at Publisher] [DOI] [Google Scholar]
15. Xiang YT, Yu X, Ungvari GS, Correll CU, Chiu HFK. Outcomes of SARS survivors in China: not only physical and psychiatric co-morbidities. East Asian Arch Psychiatry. 2014;24(1):37-8. [View at Publisher] [PMID] [Google Scholar]
16. von Keudell A, Koh KA, Shah SB, Harris MB, Smith M, Rodriguez EK, et al. Mental health after the Boston marathon bombing. Lancet Psychiatry. 2016;3(9):802-4. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Xiang Y-T, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Naeinian M, SHAIRI M, Sharifi M, Hadian M. To study reliability and validity for a brief measure for assessing Generalized Anxiety Disorder (GAD-7). 2011;9(1):41-50. [View at Publisher] [DOI] [Google Scholar]
20. Buysse DJ, Reynolds III CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Moghaddam JF, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Reliability and validity of the Persian version of the Pittsburgh Sleep Quality Index (PSQI-P). Sleep Breath. 2012;16(1):79-82. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Pinto‐Meza A, Serrano‐Blanco A, Penarrubia MT, Blanco E, Haro JM. Assessing depression in primary care with the PHQ‐9: can it be carried out over the telephone? J Gen Intern Med. 2005;20(8):738-42. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Dadfar M, Kalibatseva Z, Lester D. Reliability and validity of the Farsi version of the Patient Health Questionnaire-9 (PHQ-9) with Iranian psychiatric outpatients. Trends Psychiatry Psychother. 2018;40(2):144-51. [View at Publisher] [DOI] [PMID] [Google Scholar]
24. Takian A, Raoofi A, Kazempour-Ardebili S. COVID-19 battle during the toughest sanctions against Iran. Lancet (London, England). 2020;395(10229):1035-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901-907. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Li J-B, Yang A, Dou K, Wang L-X, Zhang M-C, Lin X-Q. Chinese public's knowledge, perceived severity, and perceived controllability of COVID-19 and their associations with emotional and behavioural reactions, social participation, and precautionary behaviour: a national survey. BMC Public Health. 2020;20(1):1589. [View at Publisher] [DOI] [PMID] [Google Scholar]
27. Kwok KO, Li KK, Chan HH, Yi YY, Tang A, Wei WI, et al. Community responses during the early phase of the COVID-19 epidemic in Hong Kong: risk perception, information exposure and preventive measures. Emerg Infect Dis. 2020;26(7):1575-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
28. Shahnazi H, Ahmadi-Livani M, Pahlavanzadeh B, Rajabi A, Hamrah MS, Charkazi A. Assessing preventive health behaviors from COVID-19 Based on the Health Belief Model (HBM) among people in Golestan province: A cross-sectional study in Northern Iran. 2020. [PPR: PPR155611] [View at Publisher] [DOI] [Google Scholar]
29. Moazzami B, Razavi-Khorasani N, Moghadam AD, Farokhi E, Rezaei N. COVID-19 and telemedicine: Immediate action required for maintaining healthcare providers well-being. J Clin Virol. 2020;126:104345. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |